Let the Right One In: Nudging Child Participation in Care Contexts through Norm-Creative Technology
Britta Teleman*, Anna Isaksson, Jens Nygren, and Petra Svedberg
Halmstad University, Halmstad, Sweden
This study addresses the knowledge gap concerning whether and how digital support tools can amplify children’s perspectives in care contexts while counteracting adult-centric and healthcare-grounded norms. Acknowledging the influential role and power position of care professionals, this paper explores 11 professionals’ perceptions of how a digital communication tool affected child participation in pediatric and social care meetings. Professionals’ narratives were analysed from a socio-technical perspective using Interpretive Description. We found that the tool’s affordances and materiality were perceived to improve the participation conditions for some children, though not all. In cases where professionals felt the tool helped facilitate participation, they described how conversing through the tool influenced topics, meeting dynamics, and parental involvement. Based on these experiences, professionals identified shortcomings in current approaches and practices, expressed an increased openness toward new tools, and ideated alternative ways of working. We discuss how design, affordances, and materiality were perceived to facilitate immediate participation, and what implications these experiences may have for norm transformation in care contexts over time. The insights can inform designers and care professionals aiming to enhance child participation in care settings.
Keywords – Care, Children, Digital Communication Tools, Norm Creativity, Norm Critique, Participation.
Relevance to Design Practice – This paper provides insights for designers in care settings on how tools can address power imbalances and exclusionary norms in care meetings with children. Identifying technological affordances that support both child participation and shifts in professionals’ perspectives can inform the design of inclusive support tools and care practices.
Citation: Teleman, B., Isaksson, A., Nygren, J., & Svedberg, P. (2025). Let the right on in: Nudging child participation in care contexts through norm-creative technology. International Journal of Design, 19(2), 43-56. https://doi.org/10.57698/v19i2.04
Received May 29, 2024; Accepted May 26, 2025; Published August 31, 2025
Copyright: © 2025 Teleman, Isaksson, Nygren, & Svedberg. Copyright for this article is retained by the authors, with first publication rights granted to the International Journal of Design. All journal content is open-accessed and allowed to be shared and adapted in accordance with the Creative Commons Attribution 4.0 International (CC BY 4.0) License.
*Corresponding Author: Britta.teleman@hh.se
Britta Teleman is an industrial designer and a Ph.D. candidate at the School of Health and Welfare, Halmstad University. Her research focus is on norm-critical perspectives and participatory design methodologies in care contexts. Engaging in all aspects of design, Britta has developed methods for inclusive stakeholder involvement in serious games and XR design. She is currently exploring provocative design as a care education tool, and teaches norm-critical approaches and design methodology at various universities in Sweden.
Anna Isaksson is an associate professor in sociology at the School of Health and Welfare, Halmstad University. Her research interests mainly concern how norm-critical design can enhance organizations’ work with gender equality and diversity issues and support norm-creative innovation. Anna’s research is primarily conducted in collaboration projects with stakeholders from both public and private sectors. Together, they have developed tools and standards aiming to promote more inclusive working environments, architecture, and physical environments.
Jens Nygren is a professor in health innovation at the School of Health and Welfare, Halmstad University. His research is driven by innovation, focusing on integrating research inquiries and projects related to various phases of the innovation process: needs assessment, design and development, testing and implementation, evaluation, dissemination, and commercialization. His research primarily targets organizational change, patient flows, decision support, patient involvement, and resource optimization within various forms of healthcare organizations. Collaborating with researchers, target groups, practitioners, and stakeholders from both public and private sectors, his research ensures a high level of applicability in clinical practice.
Petra Svedberg is a professor of Nursing at the School of Health and Welfare, Halmstad University, and she has a Ph.D. in medical science. She takes a special research interest in user involvement, shared decision making, and quality improvements in healthcare. The research focuses on how health innovations, in the form of interventions supported by digital services and health data analysis, can be developed, implemented, and evaluated to provide healthcare organizations with knowledge and support to achieve high-quality care and improved health outcomes for particular groups. She carries out most research projects in co-production with service users and stakeholders from the region, municipality, and companies.
Introduction
Children’s attendance has become synonymous with child participation in many care contexts, regardless of the child’s actual influence on care planning and decisions (Kennan et al., 2018). Care meetings are influenced by organizational, professional, and social norms, and child participation in these settings depends on the behavior of adult actors (Carlsson et al., 2018; Feenstra et al., 2014; Siembida et al., 2018; Virkki et al., 2015). When participation fails, a meeting becomes an asymmetric triad, or even a dyad with the professional and the parent (Van Bijleveld et al., 2021). This may consolidate dependency and exclusion for children with long-term relationships with care providers due to, e.g., chronic illness, disabilities, or social factors. Increased participation for this group is of particular importance since their lives and health are greatly affected by care decisions (Schalkers et al., 2015). Furthermore, this group is more experienced, willing, and thus often more competent to participate in care decisions than other children (Öster, 2024). Postponing their participation is risky, since they are less likely to try to speak up again if they do not feel listened to (Schalkers et al., 2015). Instead, these children should be supported to participate from a young age, despite—or rather because of—their vulnerable position. This is an area where design and care knowledge have the potential to complement each other and leverage innovation for sustainable change (Nogueira et al., 2022). The current study provides applicable knowledge for the development of norm-transformative care practices by investigating the experiences of professionals who tested a digital communication tool to facilitate child participation in pediatric and social care.
Background
Child Participation in Care Contexts—Benefits and Barriers
A backdrop to our inquiry is the obligation of care providers to comply with the right of all children to be heard in decisions that affect them (United Nations, 1989). Besides being a human and legal right (UNCRC was ratified by Sweden in 2020), the benefits of child participation include better preparation, greater control and self-esteem, less anxiety, more effective treatment, and fewer medical risks (Carlsson et al., 2018; Coyne, 2006, 2008; Gilljam et al., 2020; Runeson et al., 2007; Vis et al., 2011; Weingart et al., 2011). However, there is often a gap between care providers’ ambitions and the actual level of participation that children experience in encounters with care professionals (e.g., Van Bijleveld et al., 2014). Participation levels depend on professionals’ facilitation skills, attitudes, and subconscious beliefs (Coyne, 2008; Van Bijleveld et al., 2020; Virkki et al., 2015). Deeply rooted biomedical and pathogenic perspectives are still prevailing and reproducing norms of non-participation, where low involvement is seen as a result of a child’s inabilities rather than contextual factors (Teleman et al., 2021).
How care processes are organized in time and space may also work against child participation as they build on adult-centric structures. Conventional family-centered approaches do not clearly separate the child’s perspective from that of their parents (Coyne et al., 2016; Söderback et al., 2011), and parental presence has been identified as a key barrier by children, parents, and professionals alike (Teleman et al., 2021). Additionally, while research indicates that children believe they should be more involved (Moore & Kirk, 2010; Schalkers et al., 2015), adult actors often find it easier to turn to another adult than to try to involve a child (Van Bijleveld et al., 2014). Exclusion from decision-making may also be regarded as protection if professionals perceive that the child’s trust or capacity is lacking (Van Bijleveld et al., 2014). At the same time, children might stay quiet in the presence of their parents due to conflicts of loyalty or fears of not being believed (Van Bijleveld et al., 2021).
Tools for Increased Participation
Complying with the human rights of children means moving up the participation ladder beyond levels of being informed or consulted and towards influencing decisions and meeting agendas (Shier, 2001). Both legal and educational efforts have been made to increase child participation, but as these have not been sufficient to generate the desired levels, there have been frequent calls for practical tools that can support care professionals’ facilitation of participation (Feenstra et al., 2014; Nolas, 2011; Siembida et al., 2018; Van Bijleveld et al., 2021). Research has indicated that digital tools can be beneficial for involving children in care (Stålberg, Sandberg, Larsson et al., 2018; Vänskä et al., 2022), and that digital communication tools can enhance children’s autonomy and increase their influence on how procedures are carried out (Stålberg, Sandberg, & Söderbäck, 2018). Siedlikowski et al. (2020) found that children reported more symptoms, felt more prepared, received better information, and got more empathy from professionals when using a digital tool for expressing symptoms.
As care settings lag in terms of user-centered technological developments (Schalkers et al., 2015), the role of digital communication tools for child participation has generally been overlooked. At the same time, a digital format is not a magic wand, as all tools risk reproducing adult-centric norms. It has been shown that how tools are designed and used affects delegations, care processes, and outcomes, and also mediates what is considered normal and healthy (Frennert et al., 2022; Johnson, 2020). Since tools are designed and used within socio-technical systems consisting of structures and actors with certain interests and resources, they are rarely neutral (Callon, 1986; Johnson, 2020). Tools can thus shape behaviours and interactions when integrated into care settings (Frennert et al., 2022) and can either strengthen, weaken, or challenge norms and power relations (Bijker et al., 2012; Lidskog, 2020; MacKenzie & Wajcman, 1999). Design based on users’ lived experiences rather than biomedical models will be increasingly holistic and socially valid (Monteleone, 2018). Salutogenic and strength-based perspectives can further help pursue a focus on support, individual resources, and goals. In addition, designers have argued that critical approaches are needed to accelerate a shift from pathogenic-oriented perspectives to salutogenic person-centered perspectives (Kueh et al., 2022). Norm critique and norm-creative design are two such approaches, where norm critique concerns the problematization of excluding norms, and norm-creative design is considered a solution-oriented application of norm critique when striving for inclusive or empowering practices (Isaksson et al., 2017; Wikberg Nilsson & Jahnke, 2018). Few tools have been explicitly designed through a norm-creative approach, and knowledge is needed on how such technology may influence professionals’ perceptions of participation and norms. The tool in focus for this study aimed to counteract adult-centered and pathogenic/biomedical norms while amplifying child perspectives, and to fill the gap regarding tools that enable children to influence care discussions and decisions (Shier, 2001).
The Role of Professionals and ‘Studying Up’
The care professional is a key player in the socio-technical network that constitutes a meeting between a child and the care provider. While professionals may have limited power in their organization and are restrained in terms of time and resources, they are nevertheless “key people in bringing children’s and young people’s rights and participation from words into action” (Åkerström Kördel & Brunnberg, 2017, p. 25, authors’ translation). It has been recognized that patient empowerment [defined by WHO as gaining greater control over decisions and actions affecting one’s health (World Health Organization, 1998)] must be coupled with changes in service providers’ attitudes, skills, and behaviors (Nicolaidis et al., 2016). Unfortunately, a major challenge when trying to increase patient influence is the professionals’ perception that I do it already (Steffensen et al., 2018). Additionally, new tools require new routines, which can generate resistance (Rock & Donde, 2008) unless professionals feel involved and prepared for what is implemented (Batalden et al., 2016). This includes feeling prepared for a shift in roles when aiming for increased participation (Steffensen et al., 2018). However, it is crucial to acknowledge and challenge norms since professionals might face competing norms in relation to different actors in the care system (Nilsson et al., 2022). Steffensen et al. argue that when designing for shared decision-making, one must first address norms regarding how decisions are made and whose expertise is seen as influential. A central aspect—specifically in what Kumashiro (2015) describes as anti-oppressive pedagogy—is that the focus shifts from the marginalized Other to those in a position of power. To learn and develop in a profession, and thereby contribute to one’s own and the organization’s development, is not only about understanding something about the Other (in this case, the child), but one’s gaze must be turned towards one’s own beliefs and actions. This underlines the importance of a study like this, where our focus on professionals is a way of studying up and exploring how norms and power may be challenged instead of reproduced (Scambler, 2013; Stoudt et al., 2012; Sundhall, 2017; van Anders et al., 2021). Introducing a tool can make norms visible to professionals, and their stories can offer valuable insights for norm-creative design and transformative work in the context of child participation (Kumashiro, 2015).
Objectives
Based on care professionals’ reflections we aimed to understand in which ways they experienced that child participation was affected by a digital communication tool (developed through a norm-creative and salutogenic approach), which aspects of the technology that mattered for this, and if the usage influenced their perspectives regarding norms, care structures or participation.
Study Design, Setting & Methods
The study was based on semi-structured interviews exploring the perspectives of professionals from pediatric and social care on how the communication tool Galaco Play (described below) affected participation in their meetings with children. Professionals’ narratives were analysed from a socio-technical perspective, using Interpretive Description as a qualitative methodology to find patterns in the data and identify potential changes related to the tool.
The Digital Communication Tool
The digital communication tool Galaco Play was developed by a team of health science and design researchers and pediatric rehabilitation professionals. It is a form of serious game, i.e., an application designed for a primary purpose other than entertainment, but where the appeal and accessibility are enhanced through merging serious aspects with game-like elements (Djaouti, Alvarez, & Jessel, 2011). In this case, it meant embedding serious questions in a world of avatars and vivid illustrations. Through touch-based interaction and flexible navigation between themes and scenes, the tablet app aims to prepare and support children to share their opinions, feelings, priorities, and preferences related to daily life and their care in communication with care professionals. While similar support tools exist, these are either focused on questions primarily related to specific treatments or care, such as Sisom (Arvidsson et al., 2016), or on mapping the child’s life situation, such as This is Me (Blomberg et al., 2022). The current tool covers both care and other everyday contexts. It contains a range of questions that can be used to summarize and prioritize issues to facilitate high levels of participation and shared decision-making (Shier, 2001). The tool design was informed by norm-creative, salutogenic, and strength-based perspectives. It was explicitly developed to be the child’s support and not the professionals’. Nor was it meant for learning or exercising (although many adult stakeholders wished for this). The design process involved interviews with both child and adult stakeholders (Teleman et al., 2021), as well as participatory persona-workshops (involving the first author) where children could contribute in non-verbal ways through image-based collages (Teleman et al., 2022). These activities were informed by participatory design approaches addressing power structures in design processes, which are particularly pressing when participants are young and vulnerable due to disabilities (Guha et al., 2008; Heary & Hennessy, 2002; Larsson et al., 2018; Nygren et al., 2017). The workshops’ image cards and templates were aligned with existing communication support, but with new illustrations and minimizing norm-affirming images. Children used these together with pens, scissors, and glue to create their characters. To mitigate power imbalances, facilitators considered child-adult ratios for each activity and avoided power dressing. Child input was analyzed separately since it could have been overshadowed by the extensive and more articulate data from professionals and parents, and to keep track of whose perspective fed into the design (Teleman et al., 2022).
The app uses question-based elements (Figure 1). Within a space-themed world, the user selects a gender-neutral avatar and explores different planets that represent themes such as School, Home, My space, Body & Emotions, Care, Fears, and My Answers. An additional planet is solely dedicated to play. Themes can be customized, and each planet has a variety of scenes with questions based on previously validated research items and the input from interviews and workshops. My Answers is an overview of the user’s input with the possibility to note important issues. Questions can both be read and listened to and are answered with smileys. Alternatively, emotion figures can be used to mark things within scenes to express feelings and emotions (Figure 1). The norm-critical and salutogenic perspectives influenced both the design and item constructions. This led to less stereotypical imagery regarding gender, family forms, and functionality, and items related to resources and goals were added. Furthermore, questions present issues as context-bound, and positive or neutral wordings are used to avoid assuming problems (Siedlikowski et al., 2020). Quick user tests of the prototype’s logic and functions were conducted before it was tested in practice. These led to adjustments in haptics, text, sound, and visuals, enhancing its overall accessibility.
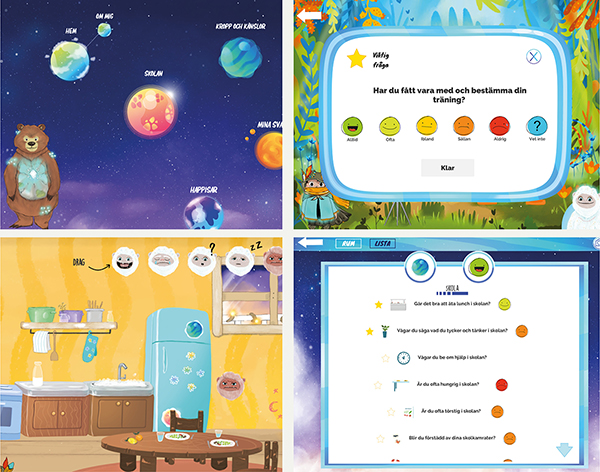
Figure 1. Screenshots from the tool prototype. Visual design by Caroline Karlsson.
Recruitment and Prototype Testing
This study involved 11 professionals from pediatric rehabilitation services, social services, and a pediatric clinic. The organizations were from different areas in the south of Sweden. All had identified the need for novel tools to increase child participation and therefore took part in a prototype testing of the digital communication tool described above. All professionals in the organization were invited to test the tool with children in their practice. The volunteering professionals were subsequently invited for interviews. All participating professionals accepted this invitation, representing seven different professions (Table 1). Ten of the 11 were women, reflecting an unequal gender representation in these professions. Ethical approval for the study was granted by the Regional Ethical Review Board at Lund University, Sweden (No: 2017/707). Written informed consent was collected from all participants, and all data were handled according to GDPR and the Swedish Ethical Review Act.
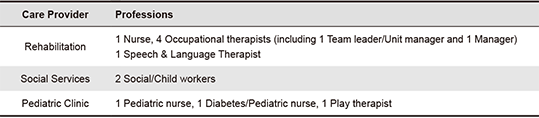
Table 1. Professions represented.
Professionals invited children they considered suitable for testing, based on the tool’s intended purpose. While the application was originally designed with and for children aged 6-17 in rehabilitation services, professionals were free to invite younger children as well. This decision was based on the understanding that age alone does not determine who may benefit from a tool, nor does it necessarily correlate with specific abilities or preferences (Clavering & McLaughlin, 2010). The professionals considered the tool accessible for some children, while too complex or less appropriate for others. This was mostly related to the app content, but a tablet was also seen as a potential distraction if there were more apps on it. Professionals selected to whom they offered the tool based on these considerations, where some were more selective than others. They also decided when and how to test it. The trial period was prolonged due to the COVID-19 pandemic and took place between January 2021 and June 2022. The prototype did not yet allow for web-based communication, so it was used at the care provider’s premises, with the professional and often one parent being present. In social services, some tests took place at the child’s home, without the parents. Professionals received an illustrated guide to the tool’s content and functions. However, many explored the tool intuitively together with the children and helped explain functions or questions when needed.
Data Collection
The interviews (30-55 minutes) were conducted and audio-recorded via Teams and Zoom in February-September 2022. The first author conducted and transcribed the interviews verbatim. A semi-structured guide with funneling themes was used, ranging from general thoughts on child participation and digital tools to experiences of the tests and new perspectives. The guide remained essentially the same throughout the data collection, although a few follow-up questions were added, concerning views on professionals’ roles in participation. All data was anonymized through coding and by replacing identifiable elements in the transcripts as well as in the quotes used to present the results.
Analysis
The data was analyzed through an Interpretive Description (ID) approach and from a socio-technical perspective. ID is a flexible, pragmatic method with roots in applied nursing science and aligned with our aim to provide applicable knowledge for the development of tools and care practices rather than theory building (Thompson Burdine et al., 2021). Using this constructivist approach, we acknowledged contextual influences and biases as well as researcher knowledge, which in this study included the first author’s experience from the industrial design field and health science training, and the second author’s social science knowledge (Hunt, 2009; Thompson Burdine et al., 2021). The general shift in design inquiry—from problem solving towards problem framing—calls for methods which are flexible enough to capture power perspectives related to tools, allow for a rethinking of stakeholders’ roles, and can describe how technology mediates and reshapes actions, relationships, and the care itself (Dankl & Akoglu, 2021; Frennert et al., 2022; Shaw & Nickpour, 2021). With this in mind, we took guidance from ID questions, including what is going on here, what mattered, and what changed, to map patterns in the data (using Word, Excel, and Keynote) and visualize changes in the network of actors (professional, child, parent) where an actant (the communication tool) was added (Hunt, 2009; Kleijberg et al., 2020; Mol, 2010).
The analysis was initiated after four interviews and then iterated, enabling a clear audit trail. Transcripts were read several times by the first and second authors, who separately highlighted quotes and added individual reflections. The first reading involved an open coding of professionals’ experiences from using the tool. The second focused on identifying potential changes in perspectives, attitudes, or relationships in the network. We then collaboratively formed categories and conceptualized the levels of change as presented in the following section. A final reading of transcripts helped to make sure no key aspects were being missed. Finally, representative quotes were selected.
Findings
This section presents the outcomes of the analysis of the interviews, addressing the inquiry into how professionals perceived that child participation was affected when testing the digital communication tool, which technological aspects that mattered, and if their experiences influenced their perspectives regarding norms and care structures related to participation. Findings will be illustrated with anonymized quotes translated from Swedish. While these findings only reflect adult narratives and focus on when there was a perceived change, our intention is not to dismiss issues of when and to whom the tool is accessible. We touch upon these issues in the discussion.
General Reflections on Change
The professionals used the communication tool in different ways with different children. It was described how using the tool changed some meetings more than others, partly due to its design and content. Many noted that the tool did not always suit the purpose of the meeting—as defined by themselves and the care plan—which also influenced their choice of when to test the tool. Many found the tool best suited for younger ages since older children might expect more advanced functions in a game. Some thought the questions posed in the tool were too vague for some children, while others considered them too narrow for other children. Professionals described how they helped skip questions regarding treatments or aids that did not apply to the child, or navigating design issues (such as that Home was pictured as just one place). They also made suggestions, e.g., that sound features could be turned off if stressful for a child, or requested pedagogic content to fit their disciplinary focus (although training was not the tool’s purpose). In cases where the tool appeared not attractive or not sufficiently accessible (based on the children’s reactions), the professionals perceived the conditions for participation as unchanged; the tool did neither increase nor decrease participation, and the roles remained the same. On the other hand, in cases where the professional perceived that the tool worked well for or suited a child, various forms of change were described. We see this change as taking place on three levels, with a directionality of the changes: when the affordances of the tool was perceived to affect the participatory conditions for a child (Level 1), it influenced the meeting dynamics and roles in the network (Level 2), which in turn elicited an awareness where professionals problematised current practices, identified needs for development, and ideated new ways of working (Level 3). Figure 2 illustrates how change either did not take place (unchanged conditions) or took place on the three levels as defined in the coloured boxes. The following sections describe these changes in further detail.
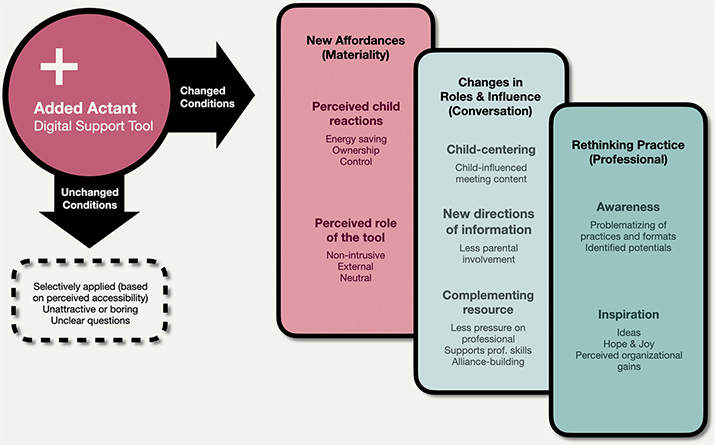
Figure 2. Introducing the tool led to either unchanged conditions or changes on three levels.
Level 1—New Affordances
Professionals perceived that when the tool suited the child it improved the participatory conditions beyond what they had achieved in previous meetings with more traditional tools. This had to do with the materiality and affordances of the tool. The familiar tablet format was considered more fun and was perceived to enthuse children. Its visuals, gamified logic, questions, and touch-based interaction were perceived as enabling children to create input with seemingly little effort and less adult support than in regular meetings. The professionals also perceived that it offered control, and that focusing on something external and fun saved energy:
And that child—I didn’t need to say anything. Just clicked, very much like this, click there, click there, read this, move it there... So, I think that the child was enabled to feel in control. More than when I ask questions because that’s probably very energy intensive. [This was] not like having a conversation with me about something but having something visual to focus on. Now the child could focus on this, and it was a little like playing. (P3)
Professionals also believed that the child’s input became more honest when interacting through the tool, where one example was:
We probably wouldn’t have been able to get all those questions and answers if we had just asked them out loud. It’s actually quite good to have a tablet between us when we’re doing it because then it’s not that personal and direct, when speaking through the tablet. (P8)
The tool was seen to concretize abstract subjects such as How is school? which helped facilitate reflection and highlight positive aspects of life. It sometimes came as a surprise for professionals that issues that they deemed irrelevant turned out to be key for a child, such as musings about death or the future, or that things that professionals took for granted were unclear for the child, e.g., why a child received a certain treatment. Unknown issues also emerged, which the professionals related to the differently posed questions:
What surprised me a little with this material, which I used together with a 12-year-old, was what emerged. It was someone I’d known a long time, worked with for a long time but things emerged that we had never actually talked about. That she could express thanks to these figures, the statements and the figures, it was something that worked for her. (P1)
Professionals brought up issues of ownership and integrity, and that the tool gave children the possibility to avoid face-to-face conversations with adults. The use of a tablet did not resemble traditional rehabilitation, which was appreciated. They perceived the tool as a neutral, non-intrusive actant that did not force questions upon the child: “Then the child did it without any pressure from us, and I think that was also sort of pleasant, not to be corrected when communicating” (P3). In summary, the professionals perceived that the materiality and new affordances on this level provided an easy and attractive way for some children to prepare for, reflect, and participate in conversations.
Level 2—Changes in Roles and Influence
The second level of change reflects how the communication tool functioned as a mediating actant that affected roles, relationships, and influence in the meeting. While some professionals wished to steer the topics by selecting planets or themes for a meeting, others pointed out that:
[The tool] has been created for the child and not for the care provider. […] The important thing is not that I get the information that I need but that the child gives the information that he or she wants to give. (P3)
Another expressed that “It gave the child the possibility to explore it a little and decide what he or she wanted to talk about. Unlike in another meeting, when I started with, well perhaps what I wanted to know” (P11). It was also described how “[the children] take a more active role. And that also leads to another… It provides openings for a different type of conversation.” Conversing through the tool influenced both the subjects of the conversations and the directions of information, which affected meeting dynamics. The professionals described that when parents were present, they moved to the periphery as the tool centered the child in the conversation, thereby reconfiguring the trialogue as illustrated in Figure 3. At the same time, the child’s interaction was less exposed due to the tablet’s shielding properties. The children’s digital literacy was often high, thus further reducing the need for parents to intervene:
Yes, but all the adults were… someone was accompanied by a parent, they were completely quiet, and [the child] sat by themselves and could just do stuff and reflect on things. Sometimes you might allow the child to talk a little before the parents perhaps take command, in this case it was the child who was in command. (P6)
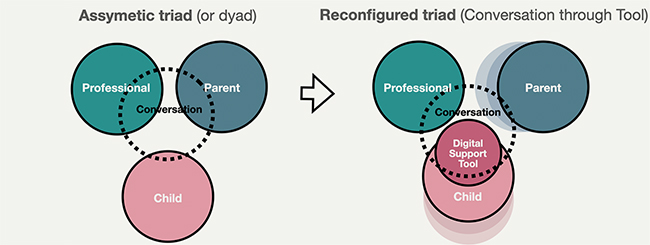
Figure 3. Changes in roles and influence (Level 2) as the tool brings the child into the conversation.
The created input was visualized, documented, and became easier to act upon (and perhaps harder to dismiss). One professional described how a child’s influence on decisions increased:
The best was that she was allowed to say something, or she could relate something that she hadn’t been able to relate before in words. Now she was able to relate it and we could talk about it afterwards. And we could discuss together, okay what are we going to do now? (P1)
The tool reduced pressure on the professional as it complemented their own skills and abilities to achieve participation. One professional claimed that:
I have probably not had to work so little in one meeting to gain so much as I did here. So, it was really great fun. And we had had contact for a long time and tried different things, but I was able to get a lot of information here. (P3)
To have a neutral, separate actant helped professionals direct the conversations and stay close to the child’s perspective. Sensitive questions appeared regardless of personal relationships and were often answered. This was seen as helpful in newly established relationships or when they found it difficult to reach a child:
I haven’t had proper contact in that way, and then it takes time before I can dig deeper and ask those questions that I was able to do when I sat together with the children with this tablet. Then it’s the tablet that determines the questions. Then it’s like I don’t have to ask them, and the children can choose I’d like to answer this question, I don’t want to answer that one for example. (P9)
It was also seen as alliance building to have a tool between oneself and the child. Professionals could make use of its novelty and discover it together. To giggle at functional flaws or irrelevant questions could be icebreaking and an opportunity to bond. The changed conditions on Level 1 were thus seen as influencing child-centering and information-sharing, while complementing the professionals’ resources and skills.
Level 3—Rethinking Practice
The third level captures how the perceived changes on previous levels—in affordances, roles, and influence—generated change beyond the instant participation in the meeting. During the interviews, the professionals problematized current meeting formats and ideated how more children would find it attractive to participate and influence their care. They identified needs for both individual and organizational development. Some expressed that they had become more open to new tools and technologies since the tests conveyed what had previously been missed, or what existing approaches were lacking. How the questions facilitated conversations was described as eye-opening by one professional:
A bit like “Wow, Oh!” that you still get a—“We don’t think in the same way.” And it’s quite cool to still get that. Because I think we sometimes believe and think that yes, I work with that, I’m quite good at it. But then like this—No, we can always be better and especially when it becomes so obvious in some cases. So I’ve absolutely learnt that, to try take it on board. (P11)
The professionals welcomed the digital format as a complement to existing tools, arguing that:
It’s something that’s there in their own environment at home and they use digital tools at school as well. However, I think that we as a profession are far behind. We’re not there where the children are. We can’t provide that in all the appointments and not in all the treatments. Yes, we need to be much, much better I think. (P2)
The professionals believed that most professions in their organizations would benefit from having this type of tool. They saw a range of possibilities and highlighted the potential to reach children who had opted out of participation, were hard to reach, or had not yet formed relationships with professionals.
Feelings of inspiration, hope, surprise, and joy were expressed. Changes in perspectives occurred to some extent, where one professional expressed:
It’s hard to describe how, but it was just that we got answers that we had never got before. To ask questions in a different way, use other tools than the traditional ones. I don’t know how I can explain it, but that it isn’t always … We are so used to how we usually work in habilitation but to do it in a slightly different way. We have many of these classical habilitation questions that we just … and it’s perhaps not these we should use at all; we should perhaps do it completely differently. It’s perhaps computer games that we should do! Then I would have wished that there was one for the young people, a little youth-inspired, a bit tougher. Because they have most often … I think of those who go in an ordinary school it’s usually quite tough for them, it would be very interesting to use a digital tool with them. (P1)
Another stated that:
It’s more that it has opened up … That I see that there are possibilities, it shouldn’t take too long before there is something [digital] that we can have. It gave me a bit of hope perhaps. But also, it was such fun to see how happy the children were, they were so proud that they could do it, and … yes, they are so very used to being digital with different things or with technology. So, it’s also to get them to grow, it takes some self-confidence to dare to answer questions, I can imagine. (P4)
Others emphasized that this type of tool helps assure the quality of care, as in some cases:
When you realize that we’ve had these few [children] where you notice that oh, we’ve really missed getting it done well. There are things here that we can actually do to make their everyday lives much better. However, they aren’t many, but there are some anyway. I think it’s a good checklist to have, to see that we really do what we are supposed to, so that there aren’t any who fall through. We have now noticed that there are actually children who fall through, who don’t get, how should I say it, the right care actually. Because it’s a type of care where they participate, know what’s happening and are understood. (P8)
Some professionals highlighted how the tool could save both time and money when used for the administration, tracking, and assessment of participation. In addition, it could help new staff get started. This third level of change thus concerns both rational and emotional awareness and incentives to change.
Discussion—Implications for Design and Care Practices
Main Findings
This study addresses the knowledge gap regarding how communication tools can amplify child perspectives in care contexts while also challenging contextual norms. It provides valuable insights for designers and other stakeholders into the mechanisms of change in these settings. Acknowledging care professionals’ power position and influence on child participation, we explored 11 professionals’ reflections after testing a digital communication tool for children, developed through a norm-creative approach. We found that many experienced that the tool contributed to participation through new affordances, which affected dynamics and the nature and level of involvement of all actors in the meeting. This mitigated norms about how meetings are conducted, who is talking, and what is discussed. The professionals could identify shortcomings in their previous approaches and proposed ideas for alternative ways to involve children. The tool and its materiality served as a pivotal catalyst, igniting a process of rethinking established practices. While the tool was not perceived as accessible or attractive enough for all children in the organisations, the professionals’ rethinking of practices shows potential for norm transformation regarding child participation in these care contexts at large. We will discuss these insights in relation to tool design and care development in the following, highlighting the importance of redirecting the gaze, understanding meanings of technology and materiality, and rethinking roles.
Redirecting the Gaze
To reach levels of meaningful participation, it is not sufficient to simply compensate for individual barriers as seen from a biomedical perspective. The key to norm transformation is to redirect one’s attention and negotiate positions of power, access, structures, and practices (Kumashiro, 2015). We have described how the addition of an actant—in the form of a digital communication tool with a norm-creative design—influenced care meetings and sparked ideas in professionals that went beyond compensation. This was signified by the professionals’ problematization of how meetings are set up, for whom they are accessible, and who sets the agenda. The perceived effects of using the tool conveyed what regular meeting formats, tools, and approaches were lacking. Children who were previously considered to have opted out of participation were now envisaged as participating but on different terms. This supports arguments that we should always question the structures when children opt out, since it might be due to adult-centered structures, norms of non-participation, or boring meeting formats (Teleman et al., 2021; Vinblad et al., 2019).
The tool in question was explicitly designed to be child-centric, where children’s needs were prioritized over adult preferences. It is plausible that adult-centric norms are reproduced to a lesser extent when a design is grounded in child perspectives. The professionals’ perceptions of how this type of tool could support children are well aligned with research where children sketched their own tools; these were designed to get attention, prepare for meetings, communicate in non-verbal ways, influence agendas, and control information-sharing (Van Bijleveld et al., 2021). Designers have also argued that to increase person-centeredness through shared decision-making, it is necessary to rethink roles, control, and communication (Dankl & Akoglu, 2021). In line with this, and contrasting studies that stress the importance of personal relationships for participation (Kennan et al., 2018; Van Bijleveld et al., 2021), our participants suggested that this type of tool could facilitate participation regardless of a professional’s relationship with a particular child. This study thus uncovers the potential to create more equitable opportunities for participation, as not all children have the desire or possibility to form close relationships with professionals. While children’s voices are essential to fully understand such norm-transformations, our findings suggest that norm-creative tools can prompt a rapid shift in perspective by offering professionals both rational and emotional incentives to reconsider current practices.
Meanings of Technology and Materiality
While many care technologies tend to bypass patients’ narratives and thus undermine humanistic aspects such as dialogue (Dankl & Akoglu, 2021; Forssén et al., 2011), this study shows that precisely the opposite may be true regarding digital communication tools in the context of child participation. Replacing face-to-face conversations with interactions through digital tools may mitigate power dynamics, as argued in Cook and Bergeron’s participatory research, where interaction through an online tool enabled participants to share thoughts “without having to defend, dialogue, or develop consensus with other participants” (Cook & Bergeron, 2019, p. 6). This aspect was also present in the current study. Professionals found it relieving to divert the conversation to an external object and believed that this mode of information-sharing was less exposing for the child. This can be compared to strategies of projecting feelings onto a character or scene as used in play or arts-based tools (e.g., Van Bijleveld et al., 2021; Waite & Conn, 2011). Another distancing function of this type of tool was that the child held it physically and could to a greater extent decide what to share, when, and with whom. A tablet is a physical shield, which meant that parents could not intervene and answer the questions unless asked to. This is a major difference in terms of ownership compared to, e.g., analogue talking mats, but also to digital care technologies that are controlled by professionals (c.f., Knutz et al., 2014).
The app-on-tablet format tested in this study was chosen based on child preferences (Siedlikowski et al., 2020; Stålberg, Sandberg, Larsson et al., 2018; Stålberg, Sandberg, & Söderbäck, 2018; Vänskä et al., 2022), and given the professionals’ accounts, we doubt that the described changes would have been achieved with an analogue version. However, while young generations are generally comfortable with digital tools (Liveng, 2023; Richardson et al., 2020; Steffensen et al., 2018), children might still opt for analogue tools if they are easier to control (Davison et al., 2022; Kerin et al., 2020). Technological format, design, and content are thereby entangled. In this case, the perceived redistribution of control, together with a reduced effort from professionals, contributed to making child participation less of a detour compared to relying on parent perspectives. This way, technology can nudge norms by making the desired behavior more accessible and thus enabling small steps toward change.
Rethinking Roles
The professional power to choose what tools to use and with whom is always problematic, especially since resistance towards power sharing is a main barrier to child participation (Coyne, 2008). Fear of losing control can make professionals hesitant to try new formats or tools (Castensøe-Seidenfaden et al., 2017). Professionals in this study noted that the tool should be an option for children, not professionals. Some children started asking for it, and this was seen as an indication that this could work. Still, it requires that the child knows all alternatives, which highlights the vital role of professionals’ attitudes and readiness to try new things. Since new tools and routines always involve some effort, incentives to change are crucial. Drawing on both participatory rationales and implementation literature, we believe that if contextual norms are articulated, professionals feel assured of the gains and prepared for a shift in roles, they will be more comfortable with power sharing (Batalden et al., 2016; Bonati & Andriana, 2021; Van Bijleveld et al., 2020). Professionals in this study expressed how they went beyond their usual approach with the digital tool, which compensated for gaps in their resources and changed their facilitating role. These experiences, along with their expectations of organizational gains, may be catalyzing factors in this regard. In addition, emotional incentives in the form of inspiration, hope, surprise, and joy can make a change of practice seem worth the effort.
Since patients’ possibilities for influencing their care largely depend on support from professionals, Petit-Steeghs et al. (2020) argue that it cannot be disconnected from professionals’ work settings and psychological factors. Finding tasks meaningful and having enough information, resources, and opportunities to learn are some key factors. Our study provides an example of how novel tools may increase these factors while at the same time counteracting the barrier of parental presence for children in care. The latter does not sit as well with literature highlighting the supporting role of parents. Schalkers et al. (2015) describe how children in hospitals considered “that parents were able to remember and recall important information, complement children’s narratives, introduce things that children had forgotten to say or ask questions that children do not dare to ask themselves” and that this “contrasts with the growing tendency to let children see their medical specialist alone” (p. 2071). Nuancing this issue of support, other studies illustrate a shift in young people’s perceptions of parental presence as essential towards a preferred independence during participatory research (Kerin et al., 2020). Such a shift was particularly apparent when testing support tools, as described by Oulton et al. (2018): ”[children] liked the idea of the ‘tool’ as a game they could play before having their blood taken, rather than having to rely on their parents during the procedure” (p.10). Kennan et al. (2018) also point to how children’s perspectives get skewed when interpreted or documented by adults—whether they are independent advocates, parents, or professionals. As mentioned initially, integrity and decreased dependency on adult gatekeepers are especially valuable for children with long-term care involvement (Schalkers et al., 2015; Williamson et al., 2015). While acknowledging that a child may seek a parent’s company for various reasons, this study presents a new perspective on parental support by suggesting that many supporting functions can be transferred from parents to support tools, thereby enhancing children’s autonomy. These insights should be further explored from the perspectives of children and possibly through the framework of self-determination theory (Ryan & Deci, 2017) in order to enhance the understanding of their motivation for participation and the role of design in promoting autonomy.
Contextual Influences and Temporal Limitations
Contextual factors may have influenced our results to some degree. Declaring the interviewer’s role in the tool design to the participants created an opportunity to discuss things in the tool that had not worked well, and critical reflections were encouraged. However, it is difficult to rule out that this previous engagement influenced the degree of positive accounts from the participants. We sought feedback from participants after drafting a preliminary analysis to ensure the findings were meaningful and comprehensible to the participants, and hoped they would indicate if they saw any issues of researcher bias (Thomas, 2017; Tracy, 2010). Member reflections are often difficult to perform, and unfortunately this study was no exception. Only one response was received (affirmative of the conclusions), which was partly due to staff turnover and parental leaves. Shortening the period between interviews and member reflections may have sustained participants’ interest in continued engagement. As many professionals appreciated that research was being done on this matter and noted that some children were excited to contribute to a research project, this may have increased both professionals’ and children’s motivation to use the tool. An interview setting may also trigger critical reflection that would not necessarily have taken place in daily practice. Many participants missed collegial discussions during the tests (there were few testers in each unit, and the COVID-19 pandemic meant little collegial contact), and it is worth considering a dedicated space for collegial reflection in future norm-transformative work. While few participating professionals saw new technology as problematic on their part, some worried that their colleagues might feel differently. This could reflect that volunteering participants might represent early adopters with an interest in digital tools and/or child participation.
Furthermore, this study does not capture temporal aspects since it was a one-off when the organizations had only tested a prototype. Since the COVID-19 pandemic reduced child appointments, testing was prolonged, but some participants still said they wished they had more time for testing. Behavior and norm changes in care contexts take time (Steffensen et al., 2018), and organizational literature suggests that participation might increase (or decrease) in a spiral fashion through successive experiences that are seldom captured in research (George & Jones, 2000). Possibilities to choose modality for using one’s voice might generate individual spirals where a child grows comfortable with expressing oneself and increasingly does so (Bonati & Andriana, 2021). On the other hand, effects might fade away as a tool’s novelty wears off. One professional reflected along these lines and feared that both enthusiasm and honesty might decrease with time.
Our analysis relies on adult narratives and focuses on aspects of change, in the hope that nudged norms regarding child participation can affect many children in this context. From a tool design perspective, research is needed that explores children’s different experiences with this type of tool and also investigates cases where such tools are not considered accessible. At the same time, one tool can never suit all children, and a main contribution of digital communication tools is that they fill a diversity gap in the toolbox. Our findings emphasize the necessity of offering multiple modalities and enough space for a child’s perspective to be heard when developing holistic care approaches (Bonati & Andriana, 2021).
Acknowledgments
We thank the professionals who volunteered for this study and all the children who tested the tool. We also thank Senior Lecturer Max Kleijberg (Mälardalen University; Karolinska Institutet) for the helpful comments on earlier drafts. Finally, we gratefully acknowledge the funding from the Knowledge Foundation.
References
- Åkerström Kördel, J., & Brunnberg, E. (2017). Delaktighet-som rättighet, fenomen och vardagspraktik i hälso-och välfärdsarbete [Participation-as a right, phenomenon and everyday practice in health and welfare work]. Studentlitteratur.
- Arvidsson, S., Gilljam, B.-M., Nygren, J., Ruland, C. M., Nordby-Bøe, T., & Svedberg, P. (2016). Redesign and validation of sisom, an interactive assessment and communication tool for children with cancer. JMIR Mhealth Uhealth, 4(2), Article No. e76. https://doi.org/10.2196/mhealth.5715
- Batalden, M., Batalden, P., Margolis, P., Seid, M., Armstrong, G., Opipari-Arrigan, L., & Hartung, H. (2016). Coproduction of healthcare service. BMJ Quality & Safety, 25(7), 509-517. https://doi.org/10.1136/bmjqs-2015-004315
- Bijker, W. E., Hughes, T. P., & Pinch, T. J. (2012). The social construction of technological systems: New directions in the sociology and history of technology. MIT press.
- Blomberg, H., Östlund, G., Lindstedt, P. R., & Cürüklü, B. (2022). Children helping to co-construct a digital tool that is designed to increase children’s participation in child welfare investigations in Sweden. Qualitative Social Work, 21(2), 367-392. https://doi.org/10.1177/1473325021990864
- Bonati, M. L., & Andriana, E. (2021). Amplifying children’s voices within photovoice: Emerging inclusive education practices in Indonesia. British Journal of Learning Disabilities, 49(4), 409-423. https://doi.org/10.1111/bld.12405
- Callon, M. (1986). The sociology of an actor-network: The case of the electric vehicle. In M. Callon, J. Law, & A. Rip (Eds.), Mapping the dynamics of science and technology (pp. 19-34). Springer.
- Carlsson, I. M., Nygren, J. M., & Svedberg, P. (2018). Patient participation, a prerequisite for care: A grounded theory study of healthcare professionals’ perceptions of what participation means in a paediatric care context. Nursing Open, 5(1), 45-52. https://doi.org/10.1002/nop2.106
- Castensøe-Seidenfaden, P., Husted, G. R., Teilmann, G., Hommel, E., Olsen, B. S., & Kensing, F. (2017). Designing a self-management app for young people with type 1 diabetes: Methodological challenges, experiences, and recommendations. JMIR Mhealth and Uhealth, 5(10), Article No. e124. https://doi.org/10.2196/mhealth.8137
- Clavering, E. K., & McLaughlin, J. (2010). Children’s participation in health research: From objects to agents? Child: Care, Health and Development, 36(5), 603-611. https://doi.org/10.1111/j.1365-2214.2010.01094.x
- Cook, K., & Bergeron, K. (2019). Using group concept mapping to engage a hard-to-reach population in research: Young adults with life-limiting conditions. International Journal of Qualitative Methods, 18. https://doi.org/10.1177/1609406919891315
- Coyne, I. (2006). Consultation with children in hospital: Children, parents’ and nurses’ perspectives. Journal of Clinical Nursing, 15(1), 61-71. https://doi.org/10.1111/J.1365-2702.2005.01247.X
- Coyne, I. (2008). Children’s participation in consultations and decision-making at health service level: A review of the literature. International Journal of Nursing Studies, 45(11), 1682-1689. https://doi.org/10.1016/j.ijnurstu.2008.05.002
- Coyne, I., Hallström, I., & Söderbäck, M. (2016). Reframing the focus from a family-centred to a child-centred care approach for children’s healthcare. Journal of Child Health Care, 20(4), 494-502. https://doi.org/10.1177/1367493516642744
- Dankl, K., & Akoglu, C. (2021). Tangible care: Design as a vehicle for materializing shifting relationships between clinicians and patients. Design Issues, 37(2), 5-15. https://doi.org/10.1162/desi_a_00632
- Davison, J., Maguire, S., McLaughlin, M., & Simms, V. (2022). Involving adolescents with intellectual disability in the adaptation of self-reported subjective well-being measures: Participatory research and methodological considerations. Journal of Intellectual Disability Research, 66(7), 628-641. https://doi.org/10.1111/jir.12936
- Djaouti, D., Alvarez, J., & Jessel, J.-P. (2011). Classifying serious games: The G/P/S model. In P. Felicia (Ed.), Handbook of research on improving learning and motivation through educational games: Multidisciplinary approaches (pp. 118-136). IGI Global Scientific Publishing. http://dx.doi.org/10.4018/978-1-60960-495-0.ch006
- Feenstra, B., Boland, L., Lawson, M. L., Harrison, D., Kryworuchko, J., Leblanc, M., & Stacey, D. (2014). Interventions to support children’s engagement in health-related decisions: A systematic review. BMC Pediatr, 14, Article No. 109. https://doi.org/10.1186/1471-2431-14-109
- Forssén, A., Meland, E., Hetlevik, I., & Strand, R. (2011). Rethinking scientific responsibility. Journal of Medical Ethics, 37(5), 299-302. http://dx.doi.org/10.1136/jme.2010.038828
- Frennert, S., Petersson, L., Muhic, M., Rydenfält, C., Nymberg, V. M., Ekman, B., & Erlingsdottir, G. (2022). Materiality and the mediating roles of eHealth: A qualitative study and comparison of three cases. Digital Health, 8. https://doi.org/10.1177/20552076221116782
- George, J. M., & Jones, G. R. (2000). The role of time in theory and theory building. Journal of Management, 26(4), 657-684. https://doi.org/10.1177/014920630002600404
- Gilljam, B. M., Nygren, J. M., Svedberg, P., & Arvidsson, S. (2020). Impact of an electronic health service on child participation in pediatric oncology care: Quasiexperimental study. Journal of Medical Internet Research, 22(7), Article No. e17673. https://doi.org/10.2196/17673
- Guha, M. L., Druin, A., & Fails, J. A. (2008). Designing with and for children with special needs: An inclusionary model. In Proceedings of the 7th international conference on interaction design and children (pp. 61-64), ACM. https://doi.org/10.1145/1463689.14637
- Heary, C. M., & Hennessy, E. (2002). The use of focus group interviews in pediatric health care research. Journal of Pediatric Psychology, 27(1), 47-57. https://doi.org/10.1093/jpepsy/27.1.47
- Hunt, M. R. (2009). Strengths and challenges in the use of interpretive description: Reflections arising from a study of the moral experience of health professionals in humanitarian work. Qualitative Health Research, 19(9), 1284-1292. https://doi.org/10.1177/1049732309344612
- Isaksson, A., Börjesson, E., Gunn, M., Andersson, C., & Ehrnberger, K. (2017). Norm critical design and ethnography: Possibilities, objectives and stakeholders. Sociological Research Online, 22(4), 232-252. https://doi.org/10.1177/1360780417743168
- Johnson, E. (2020). Refracting through technologies: Bodies, medical technologies and norms. Routledge.
- Kennan, D., Brady, B., & Forkan, C. (2018). Supporting children’s participation in decision making: A systematic literature review exploring the effectiveness of participatory processes. The British Journal of Social Work, 48(7), 1985-2002. http://dx.doi.org/10.1093/bjsw/bcx142
- Kerin, L., Lynch, D., & McNicholas, F. (2020). Participatory development of a patient–clinician communication tool to enhance healthcare transitions for young people with 22q11.2. Irish Journal of Medical Science, 189, 761-769. https://doi.org/10.1007/s11845-019-02104-6
- Kleijberg, M., Ahlberg, B. M., Hilton, R., & Tishelman, C. (2020). Death, loss and community–Perspectives from children, their parents and older adults on intergenerational community-based arts initiatives in Sweden. Health & Social Care in the Community, 28(6), 2025-2036. https://doi.org/10.1111/hsc.13014
- Knutz, E., Markussen, T., Thomsen, S. M., & Ammentorp, J. (2014). Designing for democracy: Using design activism to renegotiate the roles and rights for patients. In Proceedings of the biennial international conference of Design Research Society (pp. 514-529). DRS.
- Kueh, C., Peng, F., Ely, P., & Durrant, G. (2022). A speculation for the future of service design in healthcare: Looking through the lens of a speculative service design framework. In M. A. Pfannstiel, N. Brehmer, & C. Rasche (Eds.), Service design practices for healthcare innovation (pp. 115-131). Springer. https://doi.org/10.1007/978-3-030-87273-1_6
- Kumashiro, K. K. (2015). Against common sense: Teaching and learning toward social justice (3rd ed.). Routledge. https://doi.org/10.4324/9781315765525
- Larsson, I., Staland-Nyman, C., Svedberg, P., Nygren, J. M., & Carlsson, I. M. (2018). Children and young people’s participation in developing interventions in health and well-being: A scoping review. BMC Health Services Research, 18(1), Article No. 507. https://doi.org/10.1186/s12913-018-3219-2
- Lidskog, R. (2020). Samhället utmanat? Artificiell intelligens och sociologisk kunskap [Society challenged? Artificial intelligence and sociological knowledge]. Sociologisk Forskning, 57(2), 99-120. https://doi.org/10.37062/sf.57.19591
- Liveng, A. (2023). When do health care apps potentially lead to empowerment? The centrality of eHealth literacy in the meeting between patient and digital technology. In Proceedings of the 10th Nordic health promotion research conference (p.78). Halmstad University.
- MacKenzie, D., & Wajcman, J. (1999). The social shaping of technology. Open university press.
- Mol, A. (2010). Actor-network theory: Sensitive terms and enduring tensions. Kölner Zeitschrift für Soziologie und Sozialpsychologie, 50(1), 253-269.
- Monteleone, R. (2018). Beyond participation: Empowering people with disabilities in research and design. Technology and Innovation, 20(1-2), 133-139. https://doi.org/10.21300/20.1-2.2018.133
- Moore, L., & Kirk, S. (2010). A literature review of children’s and young people’s participation in decisions relating to health care. Journal Clinical Nursing, 19(15-16), 2215-2225. https://doi.org/10.1111/j.1365-2702.2009.03161.x
- Nicolaidis, C., Raymaker, D., McDonald, K., Kapp, S., Weiner, M., Ashkenazy, E., Gerrity, M., Kripke, C., Platt, L., & Baggs, A. (2016). The development and evaluation of an online healthcare toolkit for autistic adults and their primary care providers. Journal of General Internal Medicine, 31(10), 1180-1189. https://doi.org/10.1007/s11606-016-3763-6
- Nilsson, F., Prakash, S., & Vink, J. (2022). Service design within a multiplicity logics in health care. In M. A. Pfannstiel, N. Brehmer, & C. Rasche (Eds.), Service design practices for healthcare innovation (pp. 1-21). Springer. https://doi.org/10.1007/978-3-030-87273-1_1
- Nogueira, A., Whitney, P., & Teixeira, C. (2022). Bridging Silos between design and public health. She Ji: The Journal of Design Economics and Innovation, 8(4), 431-436. https://doi.org/10.1016/j.sheji.2022.12.002
- Nolas, S. M. (2011). Reflections on the enactment of children’s participation rights through research: Between transactional and relational spaces. Children and Youth Services Review, 33(7), 1196-1202. https://doi.org/10.1016/j.childyouth.2011.02.014
- Nygren, J. M., Lindberg, S., Wärnestal, P., & Svedberg, P. (2017). Involving children with cancer in health promotive research: A case study describing why, what, and how. JMIR Research Protocols, 6(2), Article No. e19. https://doi.org/10.2196/resprot.7094
- Öster, K. (2024, October 31). Barns och vårdnadshavares rättigheter i vården [Children’s and guardians’ rights in healthcare]. 1177.se. Retrieved from https://www.1177.se/Halland/sa-fungerar-varden/var-med-och-bestam-om-din-vard/barns-och-vardnadshavares-rattigheter-i-varden/
- Oulton, K., Oldrieve, N., Bayliss, J., Jones, V., Manning, I., Shipway, L., & Gibson, F. (2018). Using participatory and creative research methods to develop and pilot an informative game for preparing children for blood tests. Arts & Health, 10(3), 227-240. https://doi.org/10.1080/17533015.2017.1392329
- Petit-Steeghs, V., Mogami-Asselin, G., Nijenkamp, M., Spoel, M., Broerse, J., & Pittens, C. (2020). Empowering patients and health professionals to address sexual health in the context of anorectal malformations and Hirschsprung’s disease. Qualitative Health Research, 30(13), 2033-2048. https://doi.org/10.1177/1049732320944653
- Richardson, S. J., Carroll, C. B., Close, J., Gordon, A. L., O’Brien, J., Quinn, T. J., Rochester, L., Sayer, A. A., Shenkin, S. D., van der Velde, N., Woo, J., & Witham, M. D. (2020). Research with older people in a world with COVID-19: Identification of current and future priorities, challenges and opportunities. Age and Ageing, 49(6), 901-906. https://doi.org/10.1093/ageing/afaa149
- Rock, D., & Donde, R. (2008). Driving organizational change with internal coaching programs: Part one. Industrial and Commercial Training, 40(1), 10-18. https://doi.org/10.1108/00197850810841594
- Runeson, I., Martenson, E., & Enskar, K. (2007). Children’s knowledge and degree of participation in decision making when undergoing a clinical diagnostic procedure. Pediatr Nursing, 33(6), 505-511.
- Ryan, R. M., & Deci, E. L. (2017). Self-determination theory: Basic psychological needs in motivation, development, and wellness. The Guilford Press. https://doi.org/10.1521/978.14625/28806
- Scambler, G. S., S. (2013). Marx, critical realism, and health inequalities. In W. C. Cockerham (Ed.), Medical sociology on the move (pp. 83-103). Springer.
- Schalkers, I., Dedding, C. W., & Bunders, J. F. (2015). ‘[I would like] a place to be alone, other than the toilet’–Children’s perspectives on paediatric hospital care in the Netherlands. Health Expectations, 18(6), 2066-2078. https://doi.org/10.1111/hex.12174
- Shaw, C., & Nickpour, F. (2021). A framework for transitioning designerly ways: Interrogating 50 years of inclusive design for paediatric mobility. Design Journal, 24(6), 977-999. https://doi.org/10.1080/14606925.2021.1981626
- Shier, H. (2001). Pathways to participation: Openings, opportunities and obligations. Children & Society, 15(2), 107-117. https://doi.org/10.1002/chi.617
- Siedlikowski, M., Rauch, F., & Tsimicalis, A. (2020). Giving children with osteogenesis imperfecta a voice: Participatory approach for the development of the interactive assessment and communication tool sisom OI. Journal of Medical Internet Research, 22(9), Article No. e17947. https://doi.org/10.2196/17947
- Siembida, E. J., Kadan-Lottick, N. S., Moss, K., & Bellizzi, K. M. (2018). Adolescent cancer patients’ perceived quality of cancer care: The roles of patient engagement and supporting independence. Patient Education and Counseling, 101(9), 1683-1689. https://doi.org/10.1016/j.pec.2018.04.002
- Söderback, M., Coyne, I., & Harder, M. (2011). The importance of including both a child perspective and the child’s perspective within health care settings to provide truly child-centred care. Journal of Child Health Care, 15(2), 99-106. https://doi.org/10.1177/1367493510397624
- Stålberg, A., Sandberg, A., Larsson, T., Coyne, I., & Söderbäck, M. (2018). Curious, thoughtful and affirmative–Young children’s meanings of participation in healthcare situations when using an interactive communication tool. Journal of Clinical Nursing, 27(1-2), 235-246. https://doi.org/10.1111/jocn.13878
- Stålberg, A., Sandberg, A., & Söderbäck, M. (2018). Child-centred care–Health professionals’ perceptions of what aspects are meaningful when using interactive technology as a facilitator in healthcare situations. Journal of Pediatric Nursing, 43, e10-e17. https://doi.org/10.1016/j.pedn.2018.07.006
- Steffensen, K., Vinter, M., Crüger, D., Dankl, K., Coulter, A., Stuart, B., & Berry, L. (2018). Lessons in integrating shared decision-making into cancer care. Journal of Oncology Practice, 14(4), 229-235. https://doi.org/10.1200/JOP.18.00019
- Stoudt, B. G., Fox, M., & Fine, M. (2012). Contesting privilege with critical participatory action research. Journal of Social Issues, 68(1), 178-193. https://doi.org/10.1111/j.1540-4560.2011.01743.x
- Sundhall, J. (2017). A political space for children? The age order and children’s right to participation. Social Inclusion, 5(3), 164-171. https://doi.org/10.17645/si.v5i3.969
- Teleman, B., Svedberg, P., Larsson, I., Karlsson, C., & Nygren, J. M. (2022). A norm-creative method for co-constructing personas with children with disabilities: Multiphase design study. Journal of Participatory Medicine, 14(1), Article No. e29743. https://doi.org/10.2196/29743
- Teleman, B., Vinblad, E., Svedberg, P., Nygren, J. M., & Larsson, I. (2021). Exploring barriers to participation in pediatric rehabilitation: Voices of children and young people with disabilities, parents, and professionals. International Journal of Environmental Research and Public Health, 18(19), 10119. https://www.mdpi.com/1660-4601/18/19/10119
- Thomas, D. R. (2017). Feedback from research participants: Are member checks useful in qualitative research? Qualitative Research in Psychology, 14(1), 23-41. https://doi.org/10.1080/14780887.2016.1219435
- Thompson Burdine, J., Thorne, S., & Sandhu, G. (2021). Interpretive description: A flexible qualitative methodology for medical education research. Medical Education, 55(3), 336-343. https://doi.org/10.1111/medu.14380
- Tracy, S. J. (2010). Qualitative quality: Eight “big-tent” criteria for excellent qualitative research. Qualitative Inquiry, 16(10), 837-851. https://doi.org/10.1177/1077800410383121
- United Nations (1989, November 20). Convention on the rights of the child. http://www.ohchr.org/en/professionalinterest/pages/crc.aspx
- van Anders, S. M., Schudson, Z. C., Beischel, W. J., Abed, E. C., Gormezano, A., & Dibble, E. R. (2021). Overempowered? Diversity-focused research with gender/sex and sexual majorities. Review of General Psychology, 26(1), 3-21. https://doi.org/10.1177/10892680211034461
- Van Bijleveld, G. G., Bunders-Aelen, J. F., & Dedding, C. W. (2020). Exploring the essence of enabling child participation within child protection services. Child & Family Social Work, 25(2), 286-293. https://doi.org/10.1111/cfs.12684
- Van Bijleveld, G. G., de Vetten, M., & Dedding, C. W. (2021). Co-creating participation tools with children within child protection services: What lessons we can learn from the children. Action Research, 19(4), 693-709. https://doi.org/10.1177/1476750319899715
- Van Bijleveld, G. G., Dedding, C. W., & Bunders-Aelen, J. F. (2014). Seeing eye to eye or not? Young people’s and child protection workers’ perspectives on children’s participation within the Dutch child protection and welfare services. Children and Youth Services Review, 47, 253-259. https://doi.org/10.1016/j.childyouth.2014.09.018
- Vänskä, N., Sipari, S., Jeglinsky, I., Lehtonen, K., & Kinnunen, A. (2022). Co-development of the CMAP book: A tool to enhance children’s participation in pediatric rehabilitation. Disability and Rehabilitation, 44(9), 1709-1719. https://doi.org/10.1080/09638288.2021.1921061
- Vinblad, E., Larsson, I., Lönn, M., Olsson, E., Nygren, J. M., & Svedberg, P. (2019). Development of a digital decision support tool to aid participation of children with disabilities in pediatric rehabilitation services: Explorative qualitative study. JMIR Formative Research, 3(4), Article No. e14493. https://doi.org/10.2196/14493
- Virkki, M., Heino-Tolonen, T., Koskimaa, T., & Paavilainen, E. (2015). Children as decision-makers in health care: An integrative review. Clinical Nursing Studies, 3(1), 47-54. https://doi.org/10.5430/cns.v3n1p47
- Vis, S. A., Strandbu, A., Holtan, A., & Thomas, N. (2011). Participation and health–A research review of child participation in planning and decision-making. Child & Family Social Work, 16(3), 325-335. https://doi.org/10.1111/j.1365-2206.2010.00743.x
- Waite, L., & Conn, C. (2011). Creating a space for young women’s voices: Using ‘participatory video drama’ in Uganda. Gender, Place and Culture, 18(1), 115-135. https://doi.org/10.1080/0966369X.2011.535297
- Weingart, S. N., Zhu, J., Chiappetta, L., Stuver, S. O., Schneider, E. C., Epstein, A. M., David-Kasdan, J. A., Annas, C. L., Fowler, Jr, F. J., & Weissman, J. S. (2011). Hospitalized patients’ participation and its impact on quality of care and patient safety. International Journal for Quality in Health Care, 23(3), 269-277. https://doi.org/10.1093/intqhc/mzr002
- World Health Organization. (1998, June 16). Health promotion glossary. Retrieved from https://www.who.int/publications/i/item/WHO-HPR-HEP-98.1
- Wikberg Nilsson, Å., & Jahnke, M. (2018). Tactics for norm-creative innovation. She Ji: The Journal of Design, Economics, and Innovation, 4(4), 375-391. https://doi.org/10.1016/J.SHEJI.2018.11.002
- Williamson, H., Griffiths, C., & Harcourt, D. (2015). Developing young person’s face IT: Online psychosocial support for adolescents struggling with conditions or injuries affecting their appearance. Health Psychology Open, 2(2). https://doi.org/10.1177/2055102915619092

