Designing for Cervical Cancer Screening in Rural Nicaragua: A Case Study in the Informal Emergence of Complex Human-Centered Service Design
Julia Kramer 1,2,*, Vivek Rao 2, and Alice M. Agogino 2
1 Department of Mechanical Engineering, University of Michigan, Ann Arbor, Michigan, USA
2 Department of Mechanical Engineering, University of California, Berkeley, Berkeley, California, USA
Global health access and delivery in low- and middle-income countries constitutes a complex challenge for service design. While previous studies have examined how human-centered design (HCD) methods can make an impact on global health challenges, how HCD is leveraged in the design and implementation of health services in global contexts remains poorly understood. In this work, we introduce a case study of an organization called Mujeres Móviles, which provides cervical cancer education, screening, and treatment in rural Nicaragua, and—grounded in more than 100 hours of field research—we trace the organization’s journey from its founding to the scale-up of its pilot program. We critically evaluate how Mujeres Móviles’ activities align with conventional HCD models, revealing a striking consistency with HCD models, despite the organization receiving no formal training or guidance in service design or HCD approaches. These findings have important implications for service design practitioners working on global health challenges and for service design theorists seeking to support designers working in complex problem spaces.
Keywords – Cervical Cancer, Designing for Low-Resource Contexts, Global Health, Human-Centered Design, Service Design.
Relevance to Design Practice – This work offers design practitioners insight into how health services are organically designed, implemented, and iterated in a complex, low-resource setting. Practitioners will find guidance and inspiration, while current approaches to traditional service design and HCD models will be simultaneously reinforced and questioned. These insights are particularly relevant for those working in global health.
Citation: Kramer, J., Rao, V., & Agogino, A. (2022). Designing for cervical cancer screening in rural Nicaragua: A case study in the informal emergence of complex human-centered service design. International Journal of Design, 16(2), 107-123. https://doi.org/10.57698/v16i2.08
Received October 24, 2020; Accepted March 23, 2022; Published August 31, 2022.
Copyright: © 2022 Kramer, Rao, & Agogino. Copyright for this article is retained by the authors, with first publication rights granted to the International Journal of Design. All journal content is open-accessed and allowed to be shared and adapted in accordance with the Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0) License.
*Corresponding Author: kramerju@umich.edu
Julia Kramer is a Research Fellow in the Department of Mechanical Engineering at the University of Michigan. She received her BS in mechanical engineering from the University of Michigan and completed her PhD in mechanical engineering and her masters in public health at the University of California, Berkeley. Her research focuses on engineering approaches to support social justice and promote equity, particularly through the development and investigation of products, services, and systems that improve access to health care in low-resource settings. She also studies and teaches human-centered design methods that support diverse participation in equity-oriented work.
Vivek Rao is a Lecturer at the Jacobs Institute for Design Innovation and the Haas School of Business, and a postdoctoral researcher in Mechanical Engineering, all at the University of California, Berkeley. His research uses tools from design theory and methodology to explore emerging technologies and complex systems. He completed his BS, MS, and PhD, all in mechanical engineering, at the University of California, Berkeley.
Alice M. Agogino is the Roscoe and Elizabeth Hughes Professor of Mechanical Engineering, emeritus, at the University of California, Berkeley. She directs the BEST Lab: Berkeley Energy and Sustainable Technologies | Berkeley Expert Systems Technology | Berkeley Emergent Space Tensegrities. She currently serves as Chair of the Development Engineering Graduate Group and Education Director of the Blum Center for Emerging Economies at the University of California, Berkeley.
Introduction
Our world faces immense challenges in global health and equity. These challenges are not simple or one-dimensional: global health is a wicked problem (Rittel & Webber, 1973), a fact that the COVID-19 crisis has both illustrated and exacerbated (Ji et al., 2020; Lazzerini et al., 2020). Global health equity demands greater access to health infrastructure and services, especially in low- and middle-income countries (LMICs) (Kim et al., 2013).
Human-centered design (HCD) has the potential to increase access to, efficacy of, and adoption of global health services, and many case studies illustrate HCD’s promise in this domain (Bazzano et al., 2017). Indeed, with the central challenge of global healthcare being a delivery challenge (Kim et al., 2013)—a service challenge—HCD is well-suited to make an impact in this space. However, little is known about how organizations delivering health services in LMICs practice HCD and service design in complex, low-resource, and complex contexts.
This work seeks to address these gaps, using an interdisciplinary approach grounded in a case study. In this paper, we first review the literature on HCD, service design, and global health. Second, we present a case study drawn from more than 100 hours of ethnographic field research, tracing the founding, evolution, and current practices of Mujeres Móviles, an organization dedicated to delivering cervical cancer care to women in rural Nicaragua. Third, we critically evaluate how Mujeres Móviles’ practices align with conventional HCD frameworks, revealing that Mujeres Móviles appears to practice many key elements of HCD, despite no formal training in such approaches. We argue that HCD appears to be an emergent practice observed within the complex challenge of cervical cancer care delivery in an LMIC.
This paper adds to the literature by providing a case study-driven analysis of how practices of HCD and service design emerge without explicit training or guidance in a complex global health context. While previous studies have examined designers’ and healthcare practitioners’ practices of HCD methods, few have explored how global health service design adheres to conventional design frameworks. Our findings offer a new avenue for further research in HCD and service design by drawing insights from efforts and theories on delivering global health outcomes in LMICs.
Background
In this section, we first review HCD and service design. We then discuss global health as a complex problem space for the application of design, outlining current approaches in applying design to global health challenges. We conclude by describing the burden of cervical cancer, the focus of our case study.
Human-Centered Design & Service Design
HCD traces its roots to Simon’s (1969) work on design as a way of thinking, a concept subsequently explored in detail by Rittel and Webber (1973), Schön (1983), Buchanan (1992), Lawson (2006), Cross (2001, 2011), and Krippendorff (2006), among others. Here, we briefly introduce HCD, service design, and their similarities.
Human-Centered Design: Theory, Practice, and Standards
Buchanan (2001) expresses that HCD “is an ongoing search for what can be done to support and strengthen the dignity of human beings as they act out their lives.” Giacomin (2014) adds that the best examples of design address the five “classical rhetorical questions”: human factors (Who); activities, tasks, and functions (What); interactivity (When); semiotics, communication, and discourse (How); and meaning (Why).
While there are many representations of HCD, in this work we draw on Beckman and Barry’s (2007) Innovation Model. Their representation of HCD consists of four steps: Observe and Notice, Frame and Reframe, Imagine and Design, and Make and Experiment (Figure 1). A design team first Observes and Notices the experiences of stakeholders, then Frames and Reframes the problem in light of these experiences to identify a meaningful design opportunity, Imagines and Designs new ideas to address the problem, and Makes and Experiments with solutions to explore if and how these ideas address the problem, ultimately iterating through the process several times.
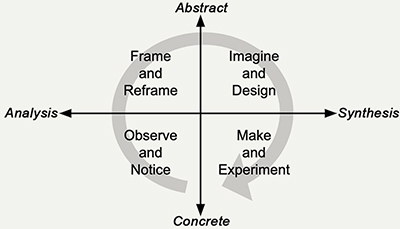
Figure 1. The Innovation Model presents HCD as a four-step process (Observe and Notice, Frame and Reframe, Imagine and Design, and Make and Experiment) laid out on two axes (analysis-synthesis and concrete-abstract). Source: adapted from (Beckman & Barry, 2007). Reused with gratis reuse permission from SAGE Publications.
Additionally, we draw upon the International Organization for Standardization’s (ISO) criteria of HCD. According to ISO 9241-210 (2010): “human-centred design is an approach to systems design and development that aims to make interactive systems more usable by focusing on the use of the system and applying human factors/ergonomics and usability knowledge and techniques.” While the standard is specifically concerned with computer-based systems, we consider its scope to include service design. This usage is appropriate, as the standard, updated in 2010, is intended to reflect a “person’s perceptions and responses resulting from the use and/or anticipated use of a product, system or service” (Miki, 2013). Here, products, systems, and services (PSS) are intentionally kept general, so as to encompass both computer-based systems and services more generally. Furthermore, ISO 9241-210 evolved from a standard describing ergonomics to interactive systems generally, and now encompasses a range of PSS (Miki, 2013), as the areas in which HCD has been applied has likewise expanded.
ISO 9241-210 puts forth six characteristics of HCD:1
- Adoption of multidisciplinary skills and perspectives
- Explicit understanding of stakeholders, tasks, and environments
- Stakeholder-centered evaluation driven/refined design
- Consideration of the whole stakeholder experience
- Involvement of stakeholders throughout design and development
- Iterative process
Human-Centered Service Design
Service design as a practice and research topic has been extant since the 1970s, when scholars were exploring ways to develop management service systems to drive organizational efficiency (Boland, 1978; Cherns, 1976; Secomandi & Snelders, 2018). Service design’s emergence as an academic discipline occurred later; Hollins and Hollins’ (G. Hollins & Hollins, 1991; W. J. Hollins, 1992) and Voss’s (1992) work are among the earliest efforts to establish it as such.
What distinguishes service design from product design? Sun (2020) highlights that service design has bifurcated into a practice-centric discussion on designing services, or service engineering in which services are the objects of design activity, and designing for service, in which the end result of design activity is a component of a larger, longer-term platform, which is also designed. Kimbell (2010), one of the key proponents of designing for service, argues that everything, including products, are part of a service. Kimbell (2009) observes that designers develop and organize artifacts, business models, relationships between people, and experiences in the course of designing a service, what Kimbell (2011) later calls “[operating] at a level of socio-material configurations or systems,” distinguishing it from other design disciplines.
Service design, like HCD, consists of a mindset, a toolset, and a process (Stickdorn et al., 2018), and is inherently multidisciplinary and participatory (Holmlid, 2012; Meroni & Sangiorgi, 2011). What distinguishes service design from HCD is its inherent need to engage what Patrício et al. (2011) call multilevel[s]. Multilevels are embodied in the key tools of service design practice today (e.g., the customer value constellation, system architectures, and service blueprints), and highlight how service design pays particular attention to the backstage processes that enable key frontstage customer activities. Uniquely, service design concerns itself explicitly with the internal activities an organization undertakes to realize participant outcomes.
Despite differing nomenclature and toolsets, and a focus on internal activities, service design and human-centered design are linked at a fundamental level. We follow Secomandi and Snelders’ (2011) contention that the interface in service design—that is, the human-to-human relationship between a service organization and the end-user—is the critical layer of service design, despite widespread methodological and research focus on service infrastructure, such as real estate, operations, and many of the aforementioned internal activities. Van der Bijl-Brouwer (2017), extending Secomandi’s work, argues that human-centered perspectives and design approaches offer a powerful lens to understand and envision human-to-human service interfaces. The author demonstrates HCD’s effectiveness in designing for complex service environments, with case studies on mental health care services and elementary education (Van der Bijl-Brouwer, 2017). Looking at policy applications, Junginger (2016) contends that service design must be integrated into policymaking, but through human-centered design.
Given these similarities and distinctions, we posit that HCD offers an effective lens for examining service design. This is because of: (1) the heavy overlap in foundational processes of HCD and service design, triangulated on the critical importance of the human-to-human interface in service design; (2) the essential focus on participants shared by both approaches; and (3) the necessarily flexible and often broad scope of the designers’ activities, what Beckman and Barry (2007) describe as framing and reframing, and what Kimbell (2011) describes as design enquiry. While HCD may not capture all elements of service design or offer quantitative metrics for certain components of service design such as cost and operations, we believe that HCD presents a highly effective lens to understand the core of service design, the interface, which is particularly important for healthcare applications. For assessment of cost and operations, additional frameworks may be necessary. However, we argue that all service design includes HCD, and HCD’s frameworks, including the Innovation Model and the ISO standard, are valuable perspectives from which to examine service design activities. Accordingly, in this paper we use evidence of HCD as an indicative signal of engagement with service design.
Global Health, Human-Centered Design, & Cervical Cancer
Despite improved global health outcomes in recent decades, especially in controlling infectious disease, persistently stark disparities in global health access and outcomes underline what Braveman (2014) discusses as global health inequity. In this work, we examine cervical cancer, a largely preventable disease that has a disproportionate impact in LMICs to illustrate health inequity. Below, we introduce cervical cancer and describe its screening and treatment, which form the focus of the service design case study in this work.
Applications of Human-Centered Design for Global Health
Global health is a complex problem space, and positively intervening in global health outcomes is a multi-faceted and multi-stakeholder challenge. As Holeman and Kane (2020) argue, global health challenges are wicked problems (Rittel & Webber, 1973), while Haffeld (2012) describes global health as a complex, adaptive system. HCD has been gaining recent traction in global health (Altman et al., 2018). Practitioners believe in HCD’s utility to understand and address human challenges. The purpose of this section is to highlight prior work applying HCD to global health challenges and to explore the complexity inherent at the intersection of design and global health.
Bazzano et al. (2017) surveyed current themes at the intersection of HCD and global health, reviewing examples from both academic research and practice. Within academic research, for example, Vechakul et al. (2015) applied HCD to “develop concepts for stimulating a vibrant local economy in the Oakland Best Babies Zone,” an initiative to reduce infant mortality inequities. Van Hoof et al. (2015) provide another academic example, applying co-design to involve bed-ridden nursing home residents in the “exploration and generation of innovative environmental enrichment scenarios.” Within the practice sphere, for example, IDEO, frog design, and Dalberg Design all engage in a portfolio of global health and wellness work. Also in practice, funding agencies and foundations have dedicated resources to supporting HCD in health, including Design for Health, a community created by the United States Agency for International Development (USAID) and the Gates Foundation to assemble funders, implementers, and designers to achieve global health goals (Design for Health, n.d.-a).
The study presented in this paper is unique in its presentation of an informally emergent example of HCD in the global health field. The examples cited above refer to applications where practitioners intentionally applied an HCD approach to a global health challenge and then documented their findings and resulting solutions. In this study, we present a case study of practitioners who did not explicitly set out to apply HCD but instead set out to address a pressing health need. We show how the practitioners in this case study unintentionally followed an HCD approach.
HCD is particularly suited to delivering global health outcomes because such outcomes fundamentally require services. Indeed, the standard term for delivering healthcare is health services, pointing to the delivery of an outcome independent of goods exchanged, as per Kimbell’s (2011) framework (Frenk, 2010). As Kim et al. (2013) argue, delivery is the determining factor in the success of healthcare interventions, and delivery is contingent on a variety of complex factors, many of them dependent on local stakeholders and systems. The focus on delivery in the success of global health interventions highlights such interventions’ nature as services. Lambe et al.’s (2020) work on service design for behavior change in LMICs highlights the power of HCD to drive positive impact in complex systems like global health.
Despite the promise of applying HCD to global health, a number of tensions exist between the two fields (Altman et al., 2018). First, there is often a difference between what stakeholders want (the concern of HCD) and what healthcare providers believe is most beneficial to stakeholders (the concern of the health field). Second, design prioritizes a full needs assessment including literature reviews, stakeholder interviews, and stakeholder observations, while practitioners in the health field tend to rely solely on literature and extant clinical evidence when developing new solutions. Third, design research often focuses on studying small samples of outliers or extreme users while health research focuses on studying large, generalizable samples of stakeholders. Fourth, design prioritizes rapid prototyping to test iterative hypotheses [“fail faster to succeed sooner” according to (Brown, 2013)] but health prioritizes research that is driven by an evidence-based hypothesis to mitigate the risk of failure, which can bring serious health consequences (Design for Health, n.d.-b). Despite these tensions, researchers, funders, and practitioners agree that there is merit to the application of HCD in global health and that health projects can be improved through HCD (Altman et al., 2018; Bazzano et al., 2017; Design for Health, n.d.-b; Holeman & Kane, 2020).
In this study, we present a novel case study of an emergent HCD process to address a pressing health need. By documenting and analyzing a case study of the design process utilized to address a global health challenge, we demonstrate that HCD practices emerged without practitioners having formal training in the approach, and we show how evaluating the design process through an HCD lens highlights areas for improvement in the design process itself.
Overview of Cervical Cancer
In this paper, we present a case study of HCD to improve the delivery of cervical cancer care. In this section, we provide a brief overview of cervical cancer. Every year, 300,000 women die from cervical cancer, and ninety percent of these deaths occur in LMICs (Bray et al., 2018; WHO, 2019). Nearly all cervical cancer cases are caused by the common sexually-transmitted infection human papillomavirus (HPV) (CDC, 2019). Half of all HPV strains are high-risk, and untreated cases of high-risk HPV can result in long-term cell changes and cancer (WHO, 2018a).
There are three facets of cervical cancer control: primary prevention, secondary screening, and treatment (WHO, 2019). In terms of primary prevention, HPV vaccines are effective at preventing many strains of HPV (Petrosky et al., 2015). In terms of secondary screening, cytology tests [i.e., the Pap smear (Mayo Clinic, 2020)], HPV DNA tests (NIH, 2019), and visual tests [e.g., visual inspection of the cervix with acetic acid (VIA) (Sauvaget et al., 2011)] are common methods to detect precancerous cervical cells. The case study in this paper focuses on the Pap smear and VIA, detailed in Figure 2. If prevention and screening are unavailable or ineffective and a person gets cervical cancer, treatment options are similar to other types of cancer treatment: surgery, chemotherapy, and radiation.
While HPV vaccination is a priority for the WHO (2002, 2014), the challenges of establishing and sustaining vaccination programs around the world make vaccination a long-term goal rather than an immediately achievable outcome (Sipp et al., 2018; Wigle et al., 2013). Additionally, HPV vaccination is most effective when administered to a person before they are sexually active, and the WHO (2018b, 2019) recommends adolescent girls (between 9 and 14 years old) as the priority group for vaccination. Thus, regardless of the status of HPV vaccination, robust cervical cancer screening programs are necessary to manage the burden of cervical cancer, and ultimately eradicate it. Screening can identify abnormal cervical cells before they become cancerous, allowing effective proactive management of the disease. However, many women lack access to cervical cancer screening, especially in LMICs, preventing them from taking advantage of its opportunity to target the disease earlier (Arbyn et al., 2011; Denny et al., 2006; Sherris et al., 2001).
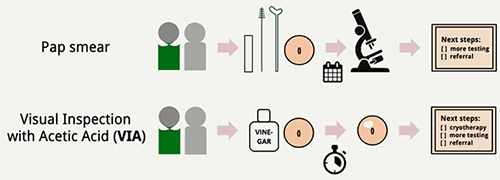
Figure 2. Steps to perform Pap smear (top) and VIA (bottom).
Pap smear: (1) healthcare provider performs pelvic examination and inserts speculum into patient’s vagina, (2) healthcare provider uses a spatula and brush to collect cells from patient’s cervix and transfers cell sample onto glass slide, (3) healthcare provider sends glass slide to laboratory where cytologist examines cells, and (4) cytologist informs healthcare provider who informs patient if precancerous cells were detected and if further testing or a referral for further care is required (Mayo Clinic, 2020).
VIA: (1) healthcare provider performs pelvic examination and inserts speculum into patient’s vagina, (2) healthcare provider inspects patient’s cervix for existing abnormalities and applies acetic acid (white vinegar) to cervix, (3) one minute after applying acetic acid, healthcare provider inspects cervix for acetowhite lesions (regions on the cervix that appear white upon application of acetic acid, signifying precancerous cells), and (4) upon visualizing acetowhite lesions, healthcare provider either performs cryotherapy to remove precancerous cells, conducts further testing, or refers patient for further care (Sauvaget et al., 2011).
In this study, we present a case study of an organization that aims to improve access to cervical cancer education, screening, and treatment in an LMIC, thereby aiming to reduce the burden of cervical cancer mortality in this setting.
Methods
A case study approach was chosen in this research for two reasons: a case study (1) lends itself to answering questions of how and why (Yin, 2014); and (2) allows researchers to holistically study the context surrounding the unit of analysis, study the dynamics present within the case setting, and combine several types of data collection to triangulate findings (Eisenhardt, 1989; Yin, 2014).
Case Selection
Mujeres Móviles was chosen as a case study based on the following criteria:
- The organization created a cervical cancer screening program in an LMIC with a high burden of cervical cancer.
- The organization’s cervical cancer screening program was active at the time of data collection.
- The organization applied a human-centered approach to design and implement their cervical cancer screening program.
After searching online and through professional networks, Author 1 identified several candidates based on these criteria. After attempting to contact more than five organizations, Author 1 successfully contacted and held preliminary conversations with two organizations, one (Mujeres Móviles) creating a novel cervical cancer screening service and one creating a novel cervical cancer screening technology (which will be the subject of a future paper). Both of these organizations were selected for inclusion, and this paper focuses on the Mujeres Móviles case study. Note that the case study selection criteria do not include formal metrics of organizational success (e.g., an impact evaluation). For the purposes of this research, we assume Mujeres Móviles (as well as the second organization, not featured in this paper) to be exemplars of organizations applying HCD to improve cervical cancer screening access. A limitation of this assumption is that we do not formally check whether either organization is successful, which will be a key area of future research; that is, to study how the process of applying HCD may contribute to the success of the designed outcomes resulting from HCD.
For confidentiality, Mujeres Móviles is a pseudonym.
Description of Mujeres Móviles
Mujeres Móviles is a non-profit organization based in Nicaragua focused on improving the holistic health of women and girls in Nicaragua. Mujeres Móviles created a mobile cervical cancer clinic to deliver cervical cancer education, screening, and treatment to women in rural Nicaragua. The mobile cervical cancer clinic consists of a truck equipped with the supplies necessary for cervical cancer education, screening, and treatment. Mujeres Móviles has two mobile cervical cancer clinics, one based in Central Nicaragua and one based in Northwestern Nicaragua.
Personnel of Mujeres Móviles
Co-Founder X is the Executive Director of Mujeres Móviles and leads clinical work. Born and raised in Nicaragua, she has training in cervical cancer screening. Before Co-Founder X graduated high school, her mother died of cervical cancer, inspiring Co-Founder X’s studies and founding of Mujeres Móviles. Co-Founder Y is the Chief Operating Officer, leading operations and collaborations for Mujeres Móviles in Nicaragua. Co-Founder Y was born and raised in the US and moved to Nicaragua in 2013. Co-Founder Z is the Chair of the Mujeres Móviles Board, working with Co-Founders X and Y to foster new collaborations and communicate with Mujeres Móviles board members. Before joining Mujeres Móviles, Co-Founder Z held leadership roles in US marketing and healthcare companies. Co-Founder Z resides in the US and coordinates with Co-Founders X and Y remotely.
Mujeres Móviles is composed of two mobile cervical cancer clinic teams. Each team consists of a clinic leader (who is trained in cervical cancer screening), two additional nurses, and a clinic operator (i.e., driver and manager of on-site logistics). The clinic leaders and nurses are women; the clinic operators are men. All members of the mobile cervical cancer clinic teams were born and raised in Nicaragua.
Five board members advise the Mujeres Móviles team on research (Board Member 1), cervical cancer screening and clinical practices (Board Member 2), education (Board Member 3), outreach and communications (Board Member 4), and non-profit management (Board Member 5).
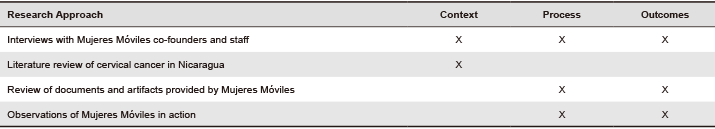
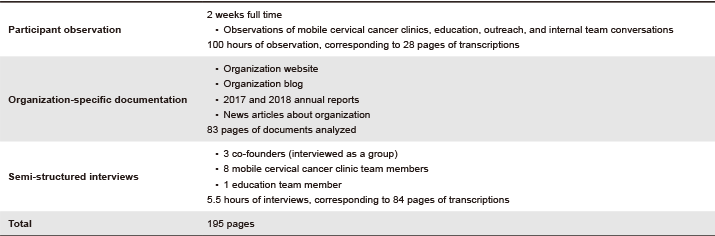
Data Collection
Data was collected in three categories: (1) the context of the cervical cancer screening program, (2) the process to create and implement the program, and (3) the outcomes of the program. Research activities were pursued to elucidate each category, as outlined in Table 1.
Table 1. Research approaches to elucidate categories of data related to the case study.
All instruments and protocols were approved by the University of California, Berkeley’s Committee for Protection of Human Subjects (protocol number 2018-10-11520).
In June 2019, Author 1 spent two weeks in Nicaragua, moving between towns in Central Nicaragua and Northwestern Nicaragua where the two main Mujeres Móviles teams are located. Participant observations (Becker & Geer, 1957) were conducted in Nicaragua for two weeks, where Author 1 shadowed Mujeres Móviles and observed their operations at the mobile cervical cancer clinics, educational events, outreach events, and internal team meetings and conversations. Organization-specific documentation was collected from Mujeres Móviles and fully transcribed for analysis, including Mujeres Móviles’ website, blog, prior annual reports, and available news articles. Semi-structured interviews were conducted with twelve members of the Mujeres Móviles organization, including all three co-founders, all eight team members of the mobile cervical cancer clinics, and one team member of the education team. The interviews ranged from twenty to ninety minutes and included the following topics:
- Respondent’s current and prior role(s) in Mujeres Móviles
- Respondent’s typical daily activities with Mujeres Móviles
- Respondent’s involvement in creating or implementing Mujeres Móviles’ services
- Respondent’s future goals with Mujeres Móviles
Interview respondents were selected such that all co-founders and mobile cervical cancer clinic team members were interviewed. The education team member was selected for an interview to provide the perspective of a Mujeres Móviles staff member not directly involved in the mobile cervical cancer clinic. Interview respondents were not compensated.
Table 2 summarizes the data collected from Mujeres Móviles. Each page of documentation corresponds to an 8.5” × 11” page consisting of content typed in 12-point font.
Table 2. Data collected with Mujeres Móviles.
Data Analysis
All participant observation notes, organization-specific documentation, and semi-structured interview transcripts listed in Table 2 were typed and de-identified. The transcripts were not sent to Mujeres Móviles, but (as described in the next paragraph) the Mujeres Móviles team reviewed the data analysis for any factual errors. After all the transcripts were typed, Author 1 and Author 2 began their analysis by coding the corpus separately and inductively using the software program MaxQDA (VERBI Software, 2018). We organized these inductive codes into themes, which included Mujeres Móviles’ phases of the design process, motivations to start or join the organization, founding and growing a healthcare organization, relationships with collaborators, team member dynamics, ways of enabling access to healthcare, and ways of navigating systems and context. These inductive codes captured Mujeres Móviles’ HCD activities plus the demographics and context of the organization. HCD activities were described by codes related to phases of the design process, to ascertain design-like behaviors and approaches observed. Similarly, service design elements were described by codes related to ways of navigating systems and context, ways of enabling access, and founding and growing a healthcare organization. These codes encompassed the critical features of service design related to the human-human interface, but also elements of the service infrastructure. We then independently coded the corpus, resolving differences in our coding along the way. At the end of this process, the 195-page corpus was coded and reviewed by two independent coders.
Then the application of codes was summarized in order to compile a description of Mujeres Móviles and their cervical cancer program. First, an overview of Mujeres Móviles was summarized, including their role within the context of the Nicaraguan healthcare system, their personnel, and the historical timeline of the organization. Next, Mujeres Móviles’ design practices used to create their cervical cancer program were summarized. Afterwards, the Mujeres Móviles team reviewed the organizational summary and the description of their design process for any factual errors, and they did not request any changes. We then analyzed the human-centeredness of Mujeres Móviles’ design approach by comparing their process to ISO 9241-210 (ISO, 2010). Finally, we compared Mujeres Móviles’ design approach to the Innovation Model (Beckman & Barry, 2007).
Case Study of Mujeres Móviles
In this section, we present a case study of Mujeres Móviles as they designed a new service to improve access to cervical cancer screening in Nicaragua. Following a brief overview of the health care context in Nicaragua, we provide a description of Mujeres Móviles, including the cervical cancer screening program the organization created and the personnel involved in the organization. We then present an analysis of how Mujeres Móviles applied HCD to create and implement their cervical cancer screening program. Then we discuss and evaluate Mujeres Móviles’ HCD process.
Context of Health in Nicaragua
Nicaragua is one of the poorest countries in the Western hemisphere (Arguello et al., 2020; BBC News, 2018). The majority of Nicaraguans live in urban areas, with the rural population dispersed across a large geographic area (Arguello et al., 2020; Sequeira et al., 2011). The health system in Nicaragua is based around the Ministry of Health (Ministerio de Salud, a.k.a. MINSA), which serves as a regulatory body and a provider of health services. MINSA consists of national hospitals and nationwide health activities; seventeen Local Comprehensive Health Care Systems (Sistemas Locales de Atención Integral de Salud, a.k.a. SILAIS), each of which includes its own departmental hospital; and local health centers, health posts, and community clinics (Sequeira et al., 2011). While Nicaraguans can access health services through MINSA for free, some Nicaraguans opt for private health facilities due to concerns about the quality of public health facilities (Mathauer et al., 2010).
A number of challenges afflict the health system in Nicaragua. First, patients’ geographic access to care is a challenge: all national hospitals are located in the capital city of Managua and, as of 2011, only three public hospitals in Nicaragua are located on the Caribbean side of the country despite this region representing over half of the total area of Nicaragua (Sequeira et al., 2011). Second, the health infrastructure does not possess consistent electricity, water, or waste management services. Third, Nicaragua faces a shortage of healthcare professionals, particularly in rural areas. Fourth, Nicaraguan health care has limited resources, with the lowest per capita health care expenditure in Central America (Sequeira et al., 2011).
Cervical cancer is the second most common cancer and the deadliest cancer among women in Nicaragua (Ferlay et al., 2018). In 2018, 21.2 per 100,000 2 women in Nicaragua were diagnosed with cervical cancer and 13.3 per 100,000 women in Nicaragua died of cervical cancer. Translated into raw numbers, 677 women in Nicaragua were diagnosed with cervical cancer and 409 women in Nicaragua died of cervical cancer in 2018.
Overview of Mobile Cervical Cancer Clinic
Mujeres Móviles created a mobile cervical cancer clinic to combine proactive outreach and sexual health education with cervical cancer screening and treatment to bring health to women in Nicaragua’s rural communities. The organization has two mobile cervical cancer clinics, each consisting of a truck equipped with the supplies necessary for cervical cancer education, screening, and treatment (Figures 3 & 4).

Figure 3. A Mujeres Móviles truck parked at a school during a mobile screening event.

Figure 4. The mobile cervical cancer clinic teams bring all the required cervical cancer screening supplies, including a gynecological table [right], cotton swabs, vinegar, and gloves.
The mobile cervical cancer clinics represent one element of Mujeres Móviles’ service delivery model. Below, we summarize the journey map presented in Figure 5.
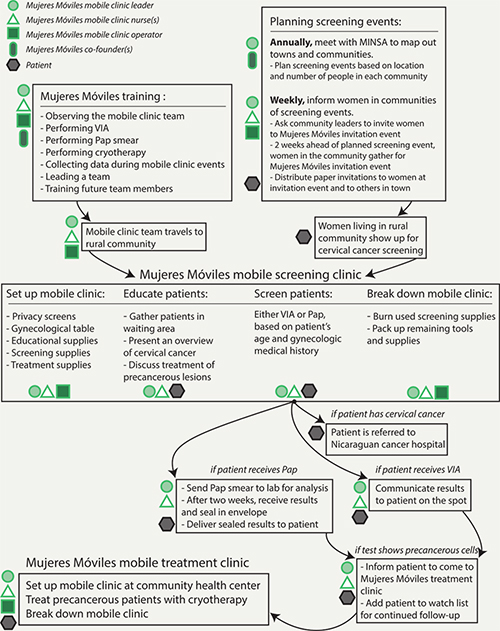
Figure 5. The journey map of Mujeres Móviles mobile cervical cancer clinics.
First, Mujeres Móviles nurses are trained to perform cervical cancer screening and treatment, and are taught key organizational processes including data collection, team leadership, and the training of new team members. Then screening events are planned in coordination with the local SILAIS. Each year, Mujeres Móviles meets with the local SILAIS to map communities in each region, plan which communities to hold screening events in, and secure permission to do so. The mobile cervical cancer clinic teams aim to visit a community once every two years.
With communities selected, Mujeres Móviles travels to perform the screening, typically arriving at a school or a health post where they establish a private screening area (Figure 4). While patients wait to be screened at the event, Mujeres Móviles nurses share information on the burden, symptoms, risk factors, and treatment of cervical cancer with them. Nurses also use the pre-screening discussion to teach patients about menstruation and breast cancer.
Patients are then screened in a private area. Depending on her age and gynecologic history, a patient receives either a Pap smear or VIA. This determination is based on Mujeres Móviles’ guidelines, developed in compliance with MINSA’s regulations. Overall, Mujeres Móviles performs Pap smears on half of patients and performs VIA on the other half. If the nurses perform VIA, they can diagnose the patient directly after the screening. If the patient exhibits precancerous lesions, the nurses inform her when the Mujeres Móviles mobile cervical cancer clinic will return to perform cryotherapy. If the nurses perform the Pap smear, they collect the patient’s cervical cells on a glass slide. During screening, if the nurses observe a serious gynecologic condition (e.g., the patient already has advanced cervical cancer), they refer the patient to a health center or departmental hospital. Approximately 5% of Mujeres Móviles’ patients receive referrals for specialized care.
When the team has finished screening all patients at the event, they re-pack their supplies, collect trash, and burn all medical waste onsite. After the screening events, Mujeres Móviles sends Pap smear samples to a cytology lab. On receipt of results, the nurses write a simple explanation of the results and follow-up steps for the patient. They deliver this information to patients in the community in a sealed envelope. Precancerous patients are added to a watch list for follow-up testing and treatment.
A cryotherapy treatment event is scheduled at least 15 days after the screening event, typically in a town’s health center. Mujeres Móviles instructs precancerous patients from the town’s surrounding communities to come for treatment. For treatment events, Mujeres Móviles teams bring their screening supplies along with cryotherapy supplies (e.g., tanks of compressed carbon dioxide and cryotherapy probes of varying sizes). Mujeres Móviles nurses perform VIA to view the precancerous lesions, and then perform cryotherapy to freeze off the lesions.
Figure 5 captures these details of Mujeres Móviles’ service delivery model.
Mujeres Móviles’ Process of Human-Centered Design
In this section, we outline Mujeres Móviles’ phases to create the mobile cervical cancer clinic (Table 3) and examine how these phases correspond to Beckman and Barry’s (2007) Innovation Model (Figure 1). We explain the specifics of Mujeres Móviles’ work in each phase, then discuss and evaluate the human-centeredness of their approach.
Table 3. The phases of Mujeres Móviles’ design process.
| Year | Phase No. | Design Phase | Description |
| 2008 | 1 | Frame and Reframe | Personal Motivation to Address Cervical Cancer. Co-Founder X’s mother in Nicaragua died of cervical cancer, inspiring Co-Founder X to address cervical cancer mortality in Nicaragua in her education and career. |
| 2013 | 2 | Observe and Notice | Observe How MINSA Provides Health Services in Rural Nicaragua. Co-Founders X and Y collaborated to transport MINSA doctors to deliver vaccinations in rural Nicaragua and observed how people living in rural areas received health services beyond the reach of many public health posts. |
| 3 | Imagine and Design | Initial Idea to Bring Cervical Cancer Screening to Rural Nicaragua. While continuing their collaboration in Phase No. 2, the co-founders envisioned a mobile cervical cancer clinic for cancer screening in rural communities, inspired by the question: “What if we could fit everything we need for screening in a suitcase?” | |
| 2014 | 4 | Observe and Notice | Background Research on Cervical Cancer Screening in Nicaragua. Based on a literature review on cervical cancer screening in low-resource settings (Co-Founder Z) and observations of cervical cancer screening at national hospitals in Managua, Nicaragua’s capital (Co-Founder X), the team identified specific gaps in MINSA’s cervical cancer screening procedures: (1) MINSA takes too long to deliver results to patients; (2) Pap smears collected suffer from quality issues and are often inconclusive; (3) elements of the health system are disconnected, which makes patient data sharing and tracking difficult; and (4) MINSA focuses on episodic health treatment instead of preventive health. Additionally, the team realized patriarchal cultural norms (machismo culture) often prevented women from prioritizing cervical cancer screening examinations. |
| 5 | Frame and Reframe | Focus on Filling In Gaps in the MINSA’s Cervical Cancer Screening. Based on their research, Mujeres Móviles committed to (1) delivering Pap smear results to patients within two weeks and (2) offering preventive cervical cancer screening to women beyond the reach of health services in Nicaragua. | |
| 6 | Observe and Notice | Conduct Initial Research with a Pilot Community. Mujeres Móviles conducted a pilot study with a rural community in Western Nicaragua to understand the viability of a mobile cervical cancer clinic and learned that community health centers were not meeting women’s needs. The community members expressed a desire for: (1) education on cervical cancer; (2) two-week turnaround on results; and (3) provision of medication and/or treatment. | |
| 7 | Imagine and Design | Envision Mobile Cervical Cancer Clinic v1. Mujeres Móviles envisioned their mobile cervical cancer screening clinic to begin with (1) an educational talk on cervical cancer and (2) screening with Pap smear, with results guaranteed within two weeks. For patients with gynecological conditions, Mujeres Móviles would work with MINSA to provide treatment. Mujeres Móviles would provide cryotherapy treatment for patients with precancerous cells. | |
| 8 | Make and Experiment | Create and Test Mobile Cervical Cancer Clinic v1. Mujeres Móviles piloted the first mobile cervical cancer clinic with the community in Western Nicaragua, screening 26 women. Mujeres Móviles learned that pre-screening education was needed to inform patients about: (1) what to expect from the Pap smear, and (2) basic human and reproductive health. Additionally, Mujeres Móviles learned of the need to treat patients with respect by: (1) considering the questions and needs of patients, and (2) performing the exam gently. | |
| 9 | Make and Experiment | Develop a Pipeline for Laboratory Analysis. The team wanted Mujeres Móviles’ Pap smear samples analyzed independently of the MINSA samples to maintain quality. Pap smear samples must be collected in a very specific way in order to be properly tested. By working with cytologists as independent contractors, Mujeres Móviles was able to obtain feedback on how they collected their Pap smears. | |
| 10 | Frame and Reframe | Focus on Addressing Holistic Women’s Health. A key takeaway from Mujeres Móviles’ pilot study in Phase 8 was the need to include holistic women’s health education. The team envisioned Mujeres Móviles’ women-centered care model as a counterpoint to Nicaragua’s dominant machismo culture, identified in Phase 4. | |
| 11 | Observe and Notice | Conduct Research on VIA. Through their literature review in Phase 4, the team learned about VIA and found that it could be very impactful in their mobile clinics because it does not depend on a cytology lab. Instead, results can be delivered directly after screening is conducted. Co-Founder X was trained in VIA in November 2014. | |
| 2015 | 12 | Make and Experiment | Launch the First Official Mujeres Móviles Event: Mobile Cervical Cancer Clinic v2. Mujeres Móviles launched mobile cervical cancer clinic v2 in Central Nicaragua. Mobile cervical cancer clinic v2 incorporated new changes including a controlled Pap smear analysis process, VIA screening, and their reframed focus on holistic women’s health. The team established a continuous improvement process, collecting feedback from patients during each screening event, which the teams use to actively refine their practices. |
| 13 | Make and Experiment | Add the Watch List to the Mobile Cervical Cancer Clinic: Mobile Cervical Cancer Clinic v3. As advised by Board Member 2, a medical doctor in Nicaragua, the team included a watch list to monitor women screened by Mujeres Móviles. The watch list categorizes women by their test results, e.g., women who need another exam in six months, women who need a hysterectomy, and women who tested negative. These categorizations help Mujeres Móviles proactively and efficiently follow up with patients. | |
| 2017 | 14 | Imagine and Design | Develop New Tools to Provide Sexual Health Education During Mobile Cervical Cancer Clinics. Due to their problem framing in Phase 10, Mujeres Móviles imagined new tools to provide holistic sexual health education. Inspired by bracelets used for family planning, Co-Founder Y wanted to use bracelets as an educational tool to teach patients about their menstrual cycle. Mujeres Móviles calls this the power bracelet, and it includes five light pink beads representing the typical number of days in menstruation, eleven white beads representing neutral days, eleven blue beads representing days of ovulation, and one bright fuchsia bead representing the day of peak fertility. A metal charm is clipped onto a different bead daily to help a woman track her menstrual cycle. |
| 15 | Make and Experiment | Add Sexual Health Education Tools to Mobile Cervical Cancer Clinic: Mobile Cervical Cancer Clinic v4. Launch Sexual Health Education in Schools. The power bracelet was launched by the mobile cervical cancer clinic team in Northwestern Nicaragua as both an explanatory prop and as a prize: while the nurses share menstrual health information with women, they give away power bracelets to women who answer questions the team posed to check for understanding. The power bracelet program is also used as part of a new program to go beyond the mobile cervical cancer clinics to teach adolescents in rural schools about sexual and reproductive health and was piloted in Central Nicaragua. | |
| 16 | Make and Experiment | Add Training to Mobile Cervical Cancer Clinic: Mobile Cervical Cancer Clinic v5. Launch Leadership Institute. At the advice of Board Member 3 who has a background in education, Mujeres Móviles launched a Leadership Institute to train young medical graduates to perform cervical cancer screening. The Leadership Institute, now its own program within Mujeres Móviles, equips nurses with the professional development skills needed to become a future leader. | |
| 2019 | 17 | Make and Experiment | Test a New Data Collection Strategy to Add to Mobile Cervical Cancer Clinic: Prepare for Mobile Cervical Cancer Clinic v6. Board Member 1, a US university professor, reached out to Mujeres Móviles about studying patients’ stress responses to receiving a precancerous diagnosis. Mujeres Móviles began collaboration with Board Member 1, improving data collection techniques: previously, the team collected data on paper, but began to pilot the use of a touch-screen tablet for data collection. |
Discussion and Evaluation of Mujeres Móviles’ Process of Human-Centered Design for Accessibility
Tracing Mujeres Móviles’ Engagement with HCD
In this section, we discuss and evaluate the HCD practices presented in Table 3.
Figure 6 shows Mujeres Móviles’ design activities mapped to the Innovation Model (Beckman & Barry, 2007) and organized into color-coded clusters. These clusters point out the high-level tasks that Mujeres Móviles carried out and demonstrate that Mujeres Móviles often worked on several overlapping tasks at once, particularly in their later phases.
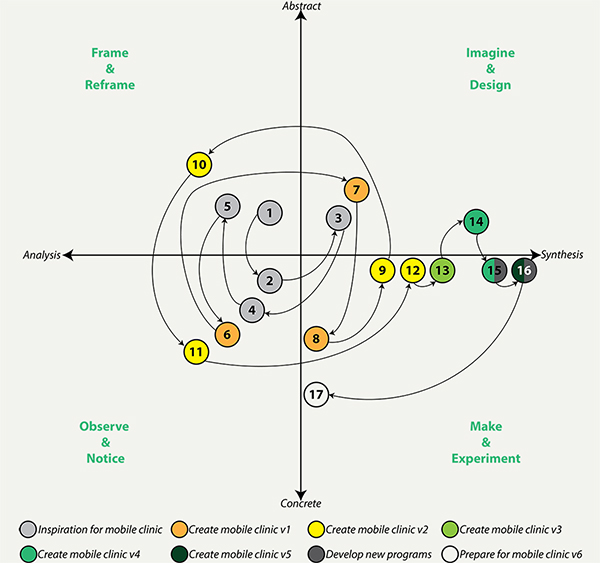
Figure 6. Mujeres Móviles’ design process.
The team followed a non-linear and iterative process. They began their project with an initial frame in mind (Phase 1) and rapidly began to observe, generate early ideas, and reframe their problem (Phases 2-5), shown in Figure 7.
After conducting initial research on cervical cancer care in Nicaragua, the team created several early versions of their mobile cervical cancer clinic (mobile clinic v1 in Phases 6-8 and mobile clinic v2 in Phases 9-12), shown in Figure 8.
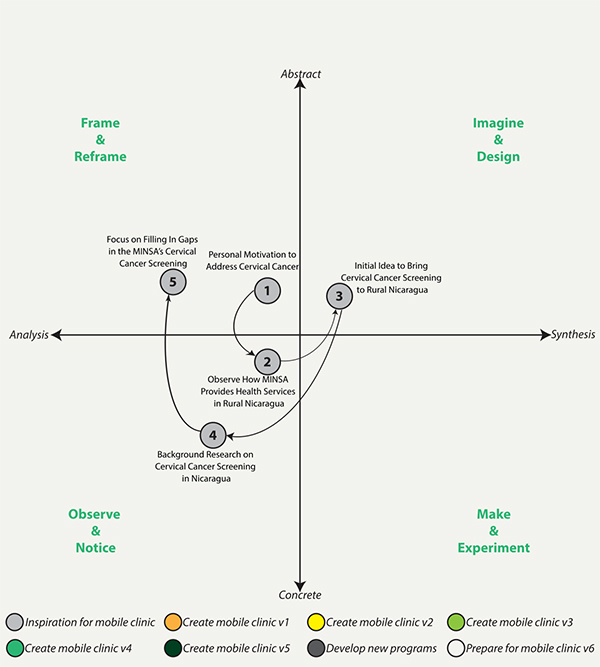
Figure 7. Mujeres Móviles’ design process: Phases 1 through 5.

Figure 8. Mujeres Móviles’ design process: Phases 6 through 12.
While creating their mobile clinic, Mujeres Móviles engaged in some ideation (Phase 7), but in general, the team engaged in much more prototyping and testing. After launching mobile clinic v2, which Mujeres Móviles considers to be their official launch, they began to rapidly iterate their mobile clinic through a series of prototypes (mobile clinic v3-v6 in Phases 13-17), shown in Figure 9. Through this process, Mujeres Móviles made a series of small “evolution[s] versus revolution[s]” (according to Co-Founder Z), focusing on continuously improving their mobile clinic through small changes.
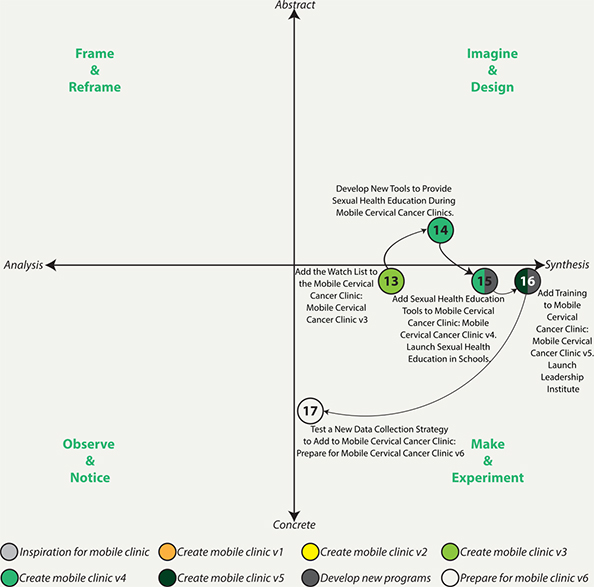
Figure 9. Mujeres Móviles’ design process: Phases 13 through 17.
Evaluating Mujeres Móviles’ Engagement with HCD
To evaluate the human-centeredness of Mujeres Móviles’ process to create their mobile cervical cancer clinic, we apply the ISO 9241-210 (2010) framework. In Table 4, we evaluate the ways in which Mujeres Móviles’ design process adheres to and diverges from each characteristic. We also provide recommendations for the Mujeres Móviles team to improve the human-centeredness of their design process going forward. Although we consider Mujeres Móviles to exhibit a comprehensive range of HCD activities and we find that Mujeres Móviles’ process to create the mobile cervical cancer clinic meets all six of the ISO HCD characteristics in some way, we note there is always room for improvement in the human-centeredness of their design process.
Table 4. Evaluation of and recommendations for improvement in the human-centeredness of the design approach employed by Mujeres Móviles to create the mobile cervical cancer clinic.
| ISO Characteristic | Mujeres Móviles’ Adherence to ISO Characteristic | Recommendations for Improvement Going Forward |
| 1. Adoption of multidisciplinary skills and perspectives | Multidisciplinary mix of clinical background (Co-Founder X), community development background (Co-Founder Y), and marketing background (Co-Founder Z). | If Mujeres Móviles were to become invested in policy development (a position they could take given their increasing work across the Nicaraguan health system), they would benefit from a governmental or health policy advisor’s perspective. |
| 2. Explicit understanding of stakeholders, tasks, and environments | Co-Founder X was born and raised in Nicaragua. Co-Founder Y has lived in Nicaragua since 2013. Co-Founder X has firsthand experience witnessing MINSA’s failure to provide adequate cervical cancer care. Co-Founder X conducted eight months of research: observing MINSA, conducting a literature review of cervical cancer screening, and learning from patients. |
This is Mujeres Móviles strongest area, so going forward they should continue to draw upon their deep subject matter expertise to design and develop new programs. As they branch into new areas (e.g., health policy), Mujeres Móviles should again conduct deep research on the stakeholders and tasks in these new environments. |
| 3. Stakeholder-centered evaluation driven/refined design | Continuous improvement allows Mujeres Móviles to refine their operations based on feedback they receive from stakeholders. | The team should consider developing an in-depth pilot study (based on the success from 2014) to either develop new ideas for the mobile cervical cancer clinic or to develop key areas of evaluation. |
| 4. Consideration of the whole stakeholder experience | Each iteration of the mobile cervical cancer clinic addresses more of the stakeholder experience, including the framing of holistic women’s health in Phase 10 (which led to the inclusion of broader sexual health education during mobile cervical cancer clinics) and the addition of the watch list in Phase 13 (which allowed Mujeres Móviles to continuously follow-up with high-risk patients). The mobile cervical cancer clinic program is an end-to-end service, starting with screening and continuing through treatment. |
The team may find that in order to address the whole stakeholder experience, they must address the whole Nicaraguan health system and the culture of patriarchy in Nicaragua. This could pose a challenge of prioritization and resource allocation, as Mujeres Móviles will need to decide how best to apply their activities to improve women’s health in Nicaragua. |
| 5. Involvement of stakeholders throughout design and development | Mujeres Móviles works with a range of stakeholders, including MINSA and SILAIS, patients, cytologists, advisors, and collaborators. Stakeholders provide feedback on the mobile cervical cancer clinic. | There is an opportunity for Mujeres Móviles to involve stakeholders to generate new ideas. Mujeres Móviles should consider ways to facilitate inspiration and collect ideas from stakeholders. |
| 6. Iterative process | Mujeres Móviles’ design process involves small and frequent iterations. The team is frequently refining their practices and adding new programs. | The content of the mobile cervical cancer clinic has not changed much since v1. Mujeres Móviles can consider testing larger transformative iterations in addition to their current smaller iterations. |
Overall, Mujeres Móviles exhibited adherence to all the ISO HCD characteristics. Mujeres Móviles particularly excelled in having an explicit understanding of stakeholders, tasks, and environments, given the time they invested in understanding the Nicaraguan health system and the needs of women seeking cervical cancer care. Throughout their work, Mujeres Móviles did not engage in highly structured idea generation or idea development, but rather engaged in these activities organically. They were able to find success in their mobile clinic due to the deep research they conducted beforehand and the iterative testing they continue to engage in. Should Mujeres Móviles choose to significantly change or add to their existing offerings (e.g., to add offerings focused on health policies in Nicaragua), the team should consider investing in another such rigorous design process. They might also add more structured idea generation processes to their approach so they can facilitate the ideas of stakeholders, which includes patients of the mobile clinics, as well as board members and advisors of Mujeres Móviles.
Implications of Mujeres Móviles’ HCD Engagement for Service Design in Complex Environments
We identify two salient implications for the broader fields of HCD and service design from this case study: the pronounced nonlinearity of the design process exhibited by Mujeres Móviles, and the emergence of HCD-like practices in the organization without formal guidance.
Service design has been acknowledged to be a nonlinear value-creation process (Morelli et al., 2021a, 2021b), as has HCD (Luchs, 2015). However, many representations of both HCD and service design present a linear sequence of steps. Our case study of Mujeres Móviles challenges this, as most clearly evidenced in Figures 7 and 8, in which the organization rapidly moves between non-sequential phases of HCD in an effort to anchor and accurately frame a problem. We posit that this nonlinearity is especially suited for service design in complex low-resource settings, such as healthcare in LMICs, because crucial phases of HCD may only be accessible through a nonlinear approach. For example, Mujeres Móviles’ pivotal reframe (the second step of Beckman and Barry’s (2007) Innovation Model) from screening for cervical cancer to delivering holistic women’s health education and services (Figure 8, Phases 6 through 12), was only made possible through the on-the-ground learning afforded by mobile clinic v1, a prototype [the fourth step of Beckman and Barry’s (2007) Innovation Model]. The lack of data and general inaccessibility of communities, combined with the complexity of the MINSA healthcare system and the agency’s relative inattention to holistic health, made prototypes and experiments the only way to challenge and refresh the team’s problem frame. In short, while previous work has established the nonlinearity of service design, we believe this nonlinearity is especially important to the effective exercise of service design in resource-constrained environments.
While we have documented the complex environment surrounding Mujeres Móviles’ service, and additionally the nonlinearity of Mujeres Móviles’ design process, this study does not claim that the complexity of the environment caused the nonlinear design process. Indeed, general guidance of design processes suggests that the design process is meant to be nonlinear (e.g., Brown, 2008). In this study, we do not presume that the complexity of Mujeres Móviles’ design challenges caused a nonlinear design process. However, the descriptive approach we have taken to document this case study is meant to show that nonlinearity was particularly salient in this design process, which emerged without the practitioners having any formal training or guidance.
As we have stated earlier, a key finding from our work is that Mujeres Móviles independently navigated their own path to delivering woman-centric healthcare services, an approach that looks remarkably similar to HCD practices. As indicated in Figures 7, 8, and 9, the team traversed the design process and showed clear evidence of all aspects of the ISO HCD standard (Table 4). This is notable because none of Mujeres Móviles’ founders or staff indicated that they had formal training in HCD, service design, or any other design innovation frameworks.
Implications for Design Practice
In the Background section, we established the key overlaps between service design and healthcare service provision. These overlaps correspond to the two approaches’ shared commitment to patient (or customer) satisfaction and the inherently interdisciplinary and integrated natures of both service design (Teixeira et al., 2012) and healthcare delivery (Lee, 2011). Therefore, while overlap between service design and a healthcare organization’s design journey is to be expected, HCD and service design practices clearly emerging in a complex, low-resource context is surprising. This finding reinforces service design models by illustrating that even in a complex context, key activities needed for the design and delivery of health services can be approximated by conventional service design models. However, this finding questions service design models for two reasons.
First, this study questions service design models because the artifacts and practices core to the practice of service design (e.g., patient journey maps, service blueprints, and the language of “touchpoints”) were not used by the Mujeres Móviles team, suggesting that team mindset and approach were significantly more effectual than the particular methods employed.
This finding—that the design mindset had a greater impact than the design methods employed—suggests that future research to evaluate learning outcomes of design students or novices should focus more on assessing shifting mindsets instead of successful application of design methods. In this vein, one area of future efforts will seek to study the role of design methods in shifting practitioners towards design mindsets.
Additionally, the importance of design mindset over design method suggests a more nuanced definition of human-centered design or service design: conducting design is not necessarily predicated on the application of design methods, but instead implies the presence of a shared mindset that seeks to fully understand the problem first, basing ideas firmly within the understanding of the problem space, and tests early versions of the solution with users, iterating from that point.
Second, this study questions service design models because, as observed in the previous section, the Mujeres Móviles team did not delve into ideation and concept development or commit appropriate resources to these important stages.
The lack of time and resources that Mujeres Móviles’ committed to ideation and concept development is not unique among health programs. The global health field may prioritize the impact of health programs on health outcomes more than the development of the program itself (Bazzano et al., 2017). This may suggest that the global health field does not prioritize the development of novel global health programs, which may help to explain the lack of time and resources committed to solution development processes. Therefore, there is an opportunity for design theorists working at the intersection of design and global health to further explore the role of creative solution development processes in developing effective health programs.
Additionally, traditional methods of concept generation in design (e.g., participatory ideation) may be challenging to effectively deliver in a complex, low-resource context like that which Mujeres Móviles faced. Therefore, there is an opportunity for design theorists to investigate other robust approaches to support the ideation efforts of organizations operating in such contexts. By investigating how to best support ideation and creative solution development in creating global health programs, theorists may discover new methods and ways of approaching ideation.
Limitations
In this study, we assume that Mujeres Móviles is an exemplar from which to build understanding of HCD and service design in global health. A limitation inherent in this assumption is that we did not conduct an impact evaluation of Mujeres Móviles, so we cannot formally assess if the organization was successful in reaching their goals. Another limitation of this work is that we collected retrospective accounts from the Mujeres Móviles team. There is likely bias in what team members recalled of their past work during their interviews with Author 1. An area of future research will be to conduct longitudinal research while a program is being designed.
As exploratory research, this work was limited to one case study. Further research on the role of HCD in creating programs to improve access to cervical cancer screening and to improve health more generally are needed. Additionally, further research is needed to study the impact of HCD on health outcomes.
Conclusions
In this paper, we examined the case study of Mujeres Móviles, documenting the organization as it created and launched a mobile cervical cancer clinic in rural Nicaragua. In the case study, we provided context on healthcare in Nicaragua and presented an overview of Mujeres Móviles and its operations. We followed Mujeres Móviles’ journey from founding to scale-up, starting with their personal inspiration in 2008; the beginning of the three co-founders working together in 2014; and continuing through June 2019 when Author 1 concluded data collection. Mujeres Móviles continues to operate today, although we did not collect any data after June 2019. We mapped Mujeres Móviles’ design process onto Beckman and Barry’s Innovation Model (2007). Finally, we applied ISO 9241-210 (2010) in order to evaluate the human-centeredness of Mujeres Móviles’ design process.
Through this evaluation, we found that Mujeres Móviles generally adhered to the criteria of HCD. The Mujeres Móviles team demonstrated particular strength by placing stakeholders in the center of their mission and design process, a focus that continued through all their iterations of the mobile clinic. There remains room for improvement in Mujeres Móviles’ HCD processes going forward. Particularly, the team should consider the next steps for their organization and develop a structured design process to move the organization forward.
We further discuss two salient insights from the case study: (1) service design practices in Mujeres Móviles’ complex, low-resource context appeared to be especially nonlinear; and (2) service design practices appeared to emerge naturally, without any formal training in Mujeres Móviles’ work to deliver healthcare, a finding that both bolsters and questions some key aspects of service design. Ultimately, the presentation of Mujeres Móviles’ process to create their mobile cervical cancer clinic provides a concrete example of how an organization on the ground is applying human-centered service design to meet their goals.
Acknowledgements
The authors sincerely thank the co-founders, staff, and beneficiaries of Mujeres Móviles for generously sharing their time during Author 1’s fieldwork. A portion of this manuscript originally appeared in Dr. Kramer’s dissertation. This work was partially funded by the National Science Foundation (DGE-1633740).
Endnotes
- 1. The original ISO 9241-210 characteristics focus on “users.” We have edited all mention of “users” to be “stakeholders,” given that this research is concerned with more than just the immediate users of a system.
- 2. The incidence rate (21.2 per 100,000) and the mortality rate (13.3 per 100,000) are both age-standardized rates.
References
- Altman, M., Huang, T. T. K., & Breland, J. Y. (2018). Design thinking in health care. Preventing Chronic Disease, 15, 180128. https://doi.org/10.5888/pcd15.180128
- Arbyn, M., Castellsagué, X., de Sanjosé, S., Bruni, L., Saraiya, M., Bray, F., & Ferlay, J. (2011). Worldwide burden of cervical cancer in 2008. Annals of Oncology, 22(12), 2675-2686. https://doi.org/10.1093/annonc/mdr015
- Arguello, R., Nietschmann, B., Orozco, M. S., Parker, F. D., & Walker, T. W. (2020). Nicaragua. Encyclopædia Britannica. https://www.britannica.com/place/Nicaragua
- Bazzano, A. N., Martin, J., Hicks, E., Faughnan, M., & Murphy, L. (2017). Human-centred design in global health: A scoping review of applications and contexts. PLOS ONE, 12(11), e0186744. https://doi.org/10.1371/journal.pone.0186744
- BBC News. (2018, May 31). Nicaragua profile–Timeline. BBC News. https://www.bbc.com/news/world-latin-america-19909695
- Becker, H., & Geer, B. (1957). Participant observation and interviewing: A comparison. Human Organization, 16(3), 28-32. https://doi.org/10.17730/humo.16.3.k687822132323013
- Beckman, S. L., & Barry, M. (2007). Innovation as a learning process: Embedding design thinking. California Management Review, 50(1), 25-56. https://doi.org/10.2307/41166415
- Boland, R. J. (1978). The process and product of system design. Management Science, 24(9), 887-898. https://doi.org/10.1287/mnsc.24.9.887
- Braveman, P. (2014). What are health disparities and health equity? We need to be clear. Public Health Reports, 129(Suppl 2), 5-8. https://doi.org/10.1177/00333549141291S203
- Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 68(6), 394-424. https://doi.org/10.3322/caac.21492
- Brown, T. (2008). Design thinking. Harvard Business Review, 86(6), 84-92.
- Brown, T. (2013, October 30). Why you should talk less and do more. IDEO design thinking. https://designthinking.ideo.com/blog/why-you-should-talk-less-and-do-more
- Buchanan, R. (1992). Wicked problems in design thinking. Design Issues, 8(2), 5-21. https://doi.org/10.2307/1511637
- Buchanan, R. (2001). Human dignity and human rights: Thoughts on the principles of human-centered design. Design Issues, 17(3), 35-39. https://doi.org/10.1162/074793601750357178
- Centers for Disease Control (CDC). (2019, August 20). HPV fact sheet. https://www.cdc.gov/std/hpv/stdfact-hpv.htm
- Cherns, A. (1976). The principles of sociotechnical design. Human Relations, 29(8), 783-792. https://doi.org/10.1177/
001872677602900806 - Cross, N. (2001). Designerly ways of knowing: Design discipline versus design science. Design Issues, 17(3), 49-55. https://doi.org/10.1162/074793601750357196
- Cross, N. (2011). Design thinking: Understanding how designers think and work. Berg.
- Denny, L., Quinn, M., & Sankaranarayanan, R. (2006). Chapter 8: Screening for cervical cancer in developing countries. Vaccine, 24, S71-S77. https://doi.org/10.1016/j.vaccine.2006.05.121
- Design for Health. (n.d.-a). About us. Retrieved August 15, 2022, from https://www.designforhealth.org/our-vision-community-of-practice
- Design for Health. (n.d.-b). Common principles of design & global health. Retrieved June 8, 2022, from https://www.designforhealth.org/resources/common-principles-of-design-in-global-health
- Eisenhardt, K. M. (1989). Building theories from case study research. Academy of Management Review, 14(4), 532-550. https://doi.org/10.5465/amr.1989.4308385
- Ferlay, J., Ervik, M., Lam, F., Colombet, M., Mery, L., Piñeros, M., Znaor, A., Soerjomataram, I., & Bray, F. (2018). Global cancer observatory: Cancer today. International Agency for Research on Cancer. https://gco.iarc.fr/today/
- Frenk, J. (2010). The global health system: Strengthening national health systems as the next step for global progress. PLOS Medicine, 7(1), e1000089. https://doi.org/10.1371/journal.pmed.1000089
- Giacomin, J. (2014). What is human centred design? The Design Journal, 17(4), 606-623. https://doi.org/10.2752/175630614X14056185480186
- Haffeld, J. (2012). Facilitative governance: Transforming global health through complexity theory. Global Public Health, 7(5), 452-464. https://doi.org/10.1080/17441692.2011.649486
- Holeman, I., & Kane, D. (2020). Human-centered design for global health equity. Information Technology for Development, 26(3), 477-505. https://doi.org/10.1080/02681102.2019.1667289
- Hollins, G., & Hollins, B. (1991). Total design: Managing the design process in the service sector. Pitman.
- Hollins, W. J. (1992). Design in the service industries. Design Management Journal (Former Series), 3(1), 76-82. https://doi.org/10.1111/j.1948-7169.1992.tb00591.x
- Holmlid, S. (2012). Participative; co-operative; emancipatory: From participatory design to service design. In Proceedings of the 1st nordic conference on service design and service innovation (pp. 105-118). Interaction Design Foundation.
- International Organization for Standardization (ISO). (2010). ISO 9241-210: Ergonomics of human-system interaction–Part 210: Human-centred design for interactive systems. ISO. https://www.iso.org/standard/52075.html
- Ji, Y., Ma, Z., Peppelenbosch, M. P., & Pan, Q. (2020). Potential association between COVID-19 mortality and health-care resource availability. The Lancet Global Health, 8(4), e480. https://doi.org/10.1016/S2214-109X(20)30068-1
- Junginger, S. (2016). Transforming public services by design. Routledge. https://doi.org/10.4324/9781315550183
- Kim, J. Y., Farmer, P., & Porter, M. E. (2013). Redefining global health-care delivery. The Lancet, 382(9897), 1060-1069. https://doi.org/10.1016/S0140-6736(13)61047-8
- Kimbell, L. (2009). The turn to service design. In G. Julier & L. Moor (Eds.), Design and creativity: Policy, management, and practice (pp. 157-173). Berg Publishers.
- Kimbell, L. (2010). From user-centred design to designing for service. Retrieved June 8, 2022, from http://www.lucykimbell.com/stuff/DMI2010_kimbell_draft.pdf
- Kimbell, L. (2011). Designing for service as one way of designing services. International Journal of Design, 5(2), 41-52.
- Krippendorff, K. (2006). The semantic turn a new foundation for design. Taylor & Francis.
- Lambe, F., Ran, Y., Jürisoo, M., Holmlid, S., Muhoza, C., Johnson, O., & Osborne, M. (2020). Embracing complexity: A transdisciplinary conceptual framework for understanding behavior change in the context of development-focused interventions. World Development, 126, 104703. https://doi.org/10.1016/j.worlddev.2019.104703
- Lawson, B. (2006). How designers think (4th ed.). Routledge. https://doi.org/10.4324/9780080454979
- Lazzerini, M., Barbi, E., Apicella, A., Marchetti, F., Cardinale, F., & Trobia, G. (2020). Delayed access or provision of care in Italy resulting from fear of COVID-19. The Lancet Child & Adolescent Health, 4(5), e10-e11. https://doi.org/10.1016/S2352-4642(20)30108-5
- Lee, S. (2011). Evaluating serviceability of healthcare servicescapes: Service design perspective. International Journal of Design, 5(2), 61-71.
- Luchs, M. G. (2015). A brief introduction to design thinking. In M. G. Luchs, K. S. Swan, & A. Griffin (Eds.), Design thinking (pp. 1-12). John Wiley & Sons, Ltd. https://doi.org/10.1002/9781119154273.ch1
- Mathauer, I., Cavagnero, E., Vivas, G., & Carrin, G. (2010). Health financing challenges and institutional options to move towards universal coverage in Nicaragua. Retrieved June 8, 2022, from https://www.who.int/healthsystems/topics/financing/healthreport/24Nicaragua.pdf
- Mayo Clinic. (2020, June 25). Pap smear. https://www.mayoclinic.org/tests-procedures/pap-smear/about/pac-20394841
- Meroni, A., & Sangiorgi, D. (2011). Design for services. Gower Publishing.
- Miki, H. (2013). Reconsidering the notion of user experience for human-centered design. In S. Yamamoto (Ed.), Human interface and the management of information. Information and interaction design (pp. 329-337). Springer. https://doi.org/10.1007/978-3-642-39209-2_38
- Morelli, N., de Götzen, A., & Simeone, L. (2021a). An approach to service design. In N. Morelli, A. de Götzen, & L. Simeone (Eds.), Service design capabilities (pp. 9-26). Springer. https://doi.org/10.1007/978-3-030-56282-3_2
- Morelli, N., de Götzen, A., & Simeone, L. (2021b). Service design capabilities. Springer Nature. https://doi.org/10.1007/978-3-030-56282-3
- National Institute of Health. (2019, December 20). HPV and pap testing. Retrieved June 8, 2022, from https://www.cancer.gov/types/cervical/pap-hpv-testing-fact-sheet
- Patrício, L., Fisk, R. P., Falcão e Cunha, J., & Constantine, L. (2011). Multilevel service design: From customer value constellation to service experience blueprinting. Journal of Service Research, 14(2), 180-200. https://doi.org/10.1177/1094670511401901
- Petrosky, E., Bocchini, J. A., Hariri, S., Chesson, H., Curtis, C. R., Saraiya, M., Unger, E. R., Markowitz, L. E., & Centers for Disease Control and Prevention. (2015). Use of 9-valent human papillomavirus (HPV) vaccine: Updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR. Morbidity and Mortality Weekly Report, 64(11), 300-304.
- Rittel, H. W. J., & Webber, M. M. (1973). Dilemmas in a general theory of planning. Policy Sciences, 4(2), 155-169. https://doi.org/10.1007/BF01405730
- Sauvaget, C., Fayette, J.-M., Muwonge, R., Wesley, R., & Sankaranarayanan, R. (2011). Accuracy of visual inspection with acetic acid for cervical cancer screening. International Journal of Gynecology & Obstetrics, 113(1), 14-24. https://doi.org/10.1016/j.ijgo.2010.10.012
- Schön, D. A. (1983). The reflective practitioner: How professionals think in action. Basic Books.
- Secomandi, F., & Snelders, D. (2011). The object of service design. Design Issues, 27(3), 20-34. https://doi.org/10.1162/DESI_a_00088
- Secomandi, F., & Snelders, D. (2018). Design processes in service innovation. Design Studies, 55, 1-4. https://doi.org/10.1016/j.destud.2018.01.003
- Sequeira, M., Espinoza, H., Amador, J. J., Domingo, G., Quintanilla, M., & de los Santos, T. (2011). The nicaraguan health system. Retrieved June 8, 2022, from https://path.azureedge.net/media/documents/TS-nicaragua-health-system-rpt.pdf
- Sherris, J., Herdman, C., & Elias, C. (2001). Cervical cancer in the developing world. The Western Journal of Medicine, 175(4), 231-233. https://doi.org/10.1136/ewjm.175.4.231
- Simon, H. A. (1969). The sciences of the artificial. MIT Press.
- Sipp, D., Frazer, I. H., & Rasko, J. E. J. (2018). No vacillation on HPV vaccination. Cell, 172(6), 1163-1167. https://doi.org/10.1016/j.cell.2018.02.045
- Stickdorn, M., Hormess, M. E., Lawrence, A., & Schneider, J. (2018). This is service design doing: Applying service design thinking in the real world. O’Reilly Media.
- Sun, Q. (2020). Towards a new agenda for service design research. The Design Journal, 23(1), 49-70. https://doi.org/10.1080/14606925.2019.1694808
- Teixeira, J., Patrício, L., Nunes, N. J., Nóbrega, L., Fisk, R. P., & Constantine, L. (2012). Customer experience modeling: From customer experience to service design. Journal of Service Management, 23(3), 362-376. https://doi.org/10.1108/09564231211248453
- Van der Bijl-Brouwer, M. (2017). Designing for social infrastructures in complex service systems: A human-centered and social systems perspective on service design. She Ji: The Journal of Design, Economics, and Innovation, 3(3), 183-197. https://doi.org/10.1016/j.sheji.2017.11.002
- Van Hoof, J., Wetzels, M. H., Dooremalen, A. M. C., Overdiep, R. A., Nieboer, M. E., Eyck, A. M. E., van Gorkom, P. J. L. M., Zwerts-Verhelst, E. L. M., Aarts, S., Vissers-Luijcks, C., van der Voort, C. S., Moonen, M. J. G. A., van de Vrande, H. A., van Dijck-Heinen, C. J. M. L., & Wouters, E. J. M. (2015). Exploring innovative solutions for quality of life and care of bed-ridden nursing home residents through codesign sessions. Journal of Aging Research, 2015, 1-14. https://doi.org/10.1155/2015/185054
- Vechakul, J., Shrimali, B. P., & Sandhu, J. S. (2015). Human-centered design as an approach for place-based innovation in public health: A case study from Oakland, California. Maternal and Child Health Journal, 19(12), 2552-2559. https://doi.org/10.1007/s10995-015-1787-x
- VERBI Software. (2018). MAXQDA 2018. https://www.maxqda.com/
- Voss, C. A. (1992). Measurement of innovation and design performance in services. Design Management Journal (Former Series), 3(1), 40-46. https://doi.org/10.1111/j.1948-7169.1992.tb00586.x
- Wigle, J., Coast, E., & Watson-Jones, D. (2013). Human papillomavirus (HPV) vaccine implementation in low and middle-income countries (LMICs): Health system experiences and prospects. Vaccine, 31(37), 3811-3817. https://doi.org/10.1016/j.vaccine.2013.06.016
- World Health Organization (Ed.). (2002). Cervical cancer screening in developing countries: Report of a WHO consultation. World Health Organization.
- World Health Organization. (2014). Comprehensive cervical
cancer control: A guide to essential practice. Retrieved June 8,
2022, from http://apps.who.int/iris/bitstream/10665/144785/
1/9789241548953_eng.pdf?ua=1 - World Health Organization. (2018a). Report on global sexually transmitted infection surveillance, 2018. Retrieved June 8, 2022, from https://apps.who.int/iris/bitstream/handle/10665/277258/9789241565691-eng.pdf
- World Health Organization. (2018b, March). Human papillomavirus vaccines (HPV). https://www.who.int/immunization/diseases/hpv/en/
- World Health Organization. (2019, January 24). Cervical cancer. https://www.who.int/en/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer
- Yin, R. K. (2014). Case study research: Design and methods (Fifth edition). Sage.

