Thinking beyond the Cure: A Case for Human-Centered Design in Cancer Care
Tara Mullaney1,*, Helena Pettersson 1, Tufve Nyholm1&2, and Erik Stolterman3
Umeå University, Umeå, Sweden
Norrlands University Hospital, Umeå, Sweden
Indiana University, Bloomington, USA
In this paper we explore how human-centered design can expand the solution space surrounding patient experience in healthcare, looking specifically at patient emotional wellbeing. The findings presented here are taken from our ethnographic research of cancer patients undergoing radiotherapy treatment; we investigated these individuals’ emotional experiences during their time in the treatment facility. Building upon previous findings within the field of nursing concerned with the prevalence of anxiety in cancer patients and the importance of person-centered care, we implement a human-centered design research approach to investigate the situational triggers of patient anxiety within the radiotherapy treatment experience. Through ‘quick ethnography’, we recognize that the fixation technology used within radiotherapy is a key trigger for anxiety in patients. Application of theory from the field of science and technology studies to our analysis of this technologically-mediated anxiety suggests that the fixation device confines the patient to a passive, disempowered role within its interactions due to it being embedded with the socially scripted ‘sick role’. Summarizing our insights, we find that human-centered design is capable of looking holistically at patient experience to discover new solutions spaces for mediating and preventing situational anxiety, and turning person-centered care within Radiotherapy into a pre-emptive practice instead of a responsive one.
Keywords – Person-Centered Care, Human-Centered Design, Patient Experience, Social Construction of Technology.
Relevance to Design Practice – This paper looks at the emotional impact medical technologies have upon patient experience, and proposes that human-centered design research is uniquely qualified to identify and analyze the problem of patient anxiety within healthcare.
Citation: Mullaney, T., Pettersson, H., Nyholm, T., & Stolterman, E. (2012). Thinking beyond the cure: A case for human-centered design in cancer care. International Journal of Design, 6(3), 27-39.
Received Oct. 3, 2011; Accepted Oct. 5, 2012; Published Dec. 31, 2012.
Copyright: © 2012 Mullaney, Pettersson, Nyholm, & Stolterman. Copyright for this article is retained by the authors, with first publication rights granted to the International Journal of Design. All journal content, except where otherwise noted, is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 2.5 License. By virtue of their appearance in this open-access journal, articles are free to use, with proper attribution, in educational and other non-commercial settings.
*Corresponding Author: tara.mullaney@dh.umu.se
Tara Mullaney is a PhD candidate in Industrial Design at the Umeå Institute of Design, Umeå University, Sweden. Mullaney’s research is situated at the intersection of Design, Science & Technology Studies (STS), and Nursing, where she investigates healthcare experiences, with a focus on patient-technology interactions and how design can be implemented within care environments to improve patient wellbeing and quality of life during illness.
Helena Pettersson, PhD, is a researcher at the Department of Culture & Media Studies, Umeå University. Pettersson’s research is situated in the intersection of Ethnology, Science & Technology Studies (STS) and Gender Studies. Through ethnography, Pettersson has studied cultural and social aspects of technology and science in ICT, physics and the life sciences.
Tufve Nyholm, PhD, is a researcher and physicist at the Department of Radiation Sciences, Umeå University and Norrlands University Hospital in Umeå, Sweden. Nyholm’s research spans over a wide variety of different aspects of cancer treatment and follow up of treatment response, with main focus on applications of MRI in radiotherapy.
Erik Stolterman is Professor and Department Chair at the School of Informatics, Indiana University. Stolterman’s research focuses on interaction design, the philosophy of design, information technology and society, information systems design, and the philosophy of technology. Stolterman has published his research in articles and in five books, including Thoughtful Interaction Design (MIT Press, 2004), The Design Way (ITP, 2003) and Methods-in-Action (McGraw-Hill, 2002).
Introduction
Medical technologies are designed with the intention of improving patient health, with each new development aimed at increased detection and better treatment offerings. Nevertheless, sometimes the very devices intended to improve health result in negative, even traumatic, emotional experiences for the patient. In this article, we make a case for human-centered design (HCD) research within healthcare, to study the emotional aspects of treatment and the impact that the built care environment can have upon patient wellbeing.
Drawing from a wealth of nursing research investigating cancer patients’ experiences of care, we first present nursing research showing that anxiety is a well-documented and commonly expressed emotional component of having cancer, along with findings which suggest that patient perceptions of the treatment environment and the care staff can play an important role in shaping their care experience. Within this paper, patient experience is defined as the sum of all interactions that influence patient perceptions across a continuum of care. The scope of our research is restricted to aspects of patient experience that occur solely within a radiotherapy clinic, i.e., the situational aspects of radiotherapy treatment. Analysis of nursing interventions aimed at managing patient anxiety shows that the current solution space of person-centered care (PCC) is focused on helping patients cope with their anxiety. This paper suggests that implementing a HCD approach to investigate the triggers of patient anxiety within cancer treatment can lead to a broader understanding of this problem area and its solution space.
We then present our case-study of a radiotherapy clinic at a large university hospital, where we employ ‘quick’ ethnographic methods to investigate cancer patients’ experiences of radiotherapy treatment. Using a design lens we look closely at patients’ interactions with care providers, the technology and the environment in order to identify situational sources of patient anxiety. Initial observational findings highlight the fixation device as a key technology within the radiation treatment process and patient experience. Further investigation of this technology, used to immobilize patients during radiation therapy, led to our critical analysis of it as a designed entity and its impact upon patient emotional wellbeing within this clinical setting.
Stories told by patients and the care staff, as well as images and detailed field-notes taken during our ethnographic investigation are used to highlight the negative emotional impact this technology has on patients during treatment. Using Science and Technology Studies (STS) theories about the social construction of technology, we analyze our observational findings to suggest why this particular technology elicits anxiety in patients. Going a step further, we assess how the impact of the fixation device can extend beyond creating negative emotions in the patient, to actually affecting the efficacy of the radiotherapy treatment. Based on our analysis of the fixation device, we present a brief summary of the many different ways in which design research can expand the solution space for dealing with patient anxiety within healthcare. The focus of this paper is not placed upon design solutions that have been implemented within the clinic, instead, it takes a detailed look at the process of problem identification, i.e., patient anxiety, and how HCD research can broaden the understanding of this problem and its potential solution spaces. The article ends with some reflections on the benefits of introducing a human-centered design approach to current cancer care practices.
Patient Centered Care
Evidence-based medicine is currently one of the predominant approaches within healthcare in the western world. It has been defined as an approach to healthcare that “integrates individual clinical expertise with the best available external clinical evidence from systematic research in order to ensure the best prediction of outcomes in medical treatment” (Sackett, Rosenberg, Gray, Haynes, & Richardson, 1996, p. 71). As a part of the tradition of scientific inquiry, evidence-based medicine’s approaches rely on maintaining distance between the researcher and the subject of investigation in order to reveal the ‘truth’ of what is happening, and to remain objective, neutral, and context-free (Penrod et al., 2007). The strong emphasis on clinical research in evidence-based medicine requires that doctors pay close attention to advances in diagnostic tests, prognostic markers, and the efficacy and safety of therapeutic, rehabilitative, and preventive regimens. As a result, physicians end up placing a high level of importance upon test results and measurable variables, while distancing themselves from the less measurable aspects of disease, such as patient wellbeing.
Evidence-based medical research and practice have made invaluable advances in healthcare, nonetheless, findings from a growing body of nursing research on patients experiences of illness and treatment suggest that medical care delivered solely from within this biomedical perspective is unable to generate a satisfactory, perhaps even acceptable, level of care from a patient perspective (Edvardsson, Sandman, & Rasmussen, 2006, 2008). Furthermore, individuals both within and outside of healthcare are challenging the traditional socially structured ‘sick role’ which constructs the patient as a passive recipient of medical care (Parsons, 1951). This is demonstrated by the research being conducted within nursing sciences which emphasizes the importance of patient empowerment and the need for practitioners to “understand [patients’] needs and engage in positive work with them” as means for creating a patient-centered practice (Kvåle & Bondevik, 2008, p. 582).
Currently, both healthcare professionals and administrators clearly recognize that providing person-centered care is important. PCC has been defined as the practice of valuing the person and those caring for them, treating people as individuals and thereby assessing and meeting the individual needs of patients rather than meeting the needs of staff, and creating a positive social environment in which the person can experience wellbeing (Brooker, 2007). This body of research highlights the importance of taking the subjective experience of the individual into account and emphasizes that employing a person-centered approach to care can promote patient well-being.
Illness can very often have an impact that extends beyond physiological symptoms. For cancer patients, significant psychological distress is common across all the stages of this life-threatening disease, impacting one-third to one-half of the patient population (Dale, Bilir, Han, & Meltzer, 2005; Teunissen, de Graeff, Voest, & de Haes, 2007). Anxiety in particular is a common psychological response to cancer diagnosis. Not only has it been shown to affect up to a quarter of all individuals suffering from this disease, but it has also been linked to a decrease in quality of life (Brown, Kroenke, Theobald, Wu, & Tu, 2010; Stark & House, 2000). This anxiety has many different contributing factors, ranging from situational anxiety caused by medical procedures and treatments, to psychiatric anxiety stemming from preexisting phobias that are activated by some aspects of the medical care, to name a few (Stiefel & Razavi, 1994).
The literature in the field tells us that anxiety within cancer patients is a complex emotion, with a wide variety of causes and is highly context and person-specific. Cancer treatment can provoke a mixture of positive and negative emotions, with the unpleasantness and threat of the process of treatment conflicting with hopes for a cure of the disease. Chemotherapy and radiotherapy treatment have both been directly associated with patient anxiety, and some radiotherapy research has shown that this anxiety does not necessarily diminish over time, suggesting that the ‘threatening element’ is persistent and that not all cancer patients adapt to the stresses of treatment (Andersen, Karlsson, Anderson, & Tewfik, 1984; Stark & House, 2000).
Research has shown that the anxiety generated by cancer treatment can impact quality of life in many different ways. For example, it can lead to less effective medical decision making, an increase in awareness and exacerbation of medical symptoms, and disruptions in cancer care (Andrykowski, 1990; Greer, Pirl, Park, Lynch, & Temel, 2008; Latini et al., 2007). Anxiety has also been shown to contribute to anorexia, nausea, vomiting and fatigue distinct from the pre-existing symptoms of disease, and is associated with increased recall of side effects experienced during treatment (Cameron, Levanthal, & Love, 1998; Forester, Kornfeld, & Fleiss, 1978). This anxiety has also been negatively associated with chemotherapy treatment adherence, showing that anxiety can have far reaching consequences (Greer et al., 2008). These research findings highlight the importance of recognizing and treating anxiety in cancer care, not only for the suffering caused by the disease itself, but also for its adverse effects on patients’ quality of life (Brown et al., 2010).
In a typical healthcare institution, the needs of care in cancer patients are perceived predominantly as disease modifying interventions (Nandini, Sridhar, Usharani, Kumar, & Salins, 2011). However, a growing number of health care professionals are advocating a holistic approach to cancer care. Treating patients’ physical and emotional needs is considered to be a vital part of improving current care systems. Psychosocial interventions have been one of the main solution spaces employed within nursing studies to address patient anxiety. These interventions focus around four different approaches: providing patient education about their disease, relaxation and stress management training, group support therapy, and individual support therapy (Carlson & Bultz, 2003). These interventions have been found to be helpful in alleviating emotional distress in patients and may benefit their medical outcomes.
From our design perspective, when looking at the solutions that have been implemented within nursing research to address the problem of anxiety in cancer patients, we note that these interventions are all characterized by their focus on coping techniques. The patient is given tools to help them learn how to manage their anxiety, through education, therapy, and relaxation techniques. At the same time llittle attention has been placed upon interventions that would impact the triggers of patient anxiety, especially for those suffering from situational anxiety activated by different aspects of the treatment experience. As such, we posit that design is uniquely qualified to expand the landscape of anxiety interventions within cancer care due to its human-centered focus and its ability to approach the situation with an open-minded, holistic perspective.
Design as a discipline is characterized by creating change. There are many different approaches that can be employed within the field of design, however the methodology that we employ in our research, and one that we find to match well with the patient focus of PCC, is human-centered design. HCD, also known as people-centered design or user-centered design, places emphasis upon understanding human needs and how design can respond to these needs. HCD processes focus on creating new solutions for the world, and “it begins by examining the needs, dreams, and behaviors of the people we want to affect with our solutions” (IDEO, 2011, p. 6). This paper employs an HCD research approach within the context of our case study, the radiotherapy clinic of a large university hospital, using ‘quick’ ethnographic methods to understand and problematize the cancer patient experience within this setting.
Research Approach
The research presented in this paper was conducted within the radiotherapy clinic of Norrlands University Hospital (NUS) in Umeå, Sweden, where we spent two months conducting ‘quick ethnography’ within this environment. Our research approach was structured around the ethical rules and guidelines for research set forth by the Swedish Research Council, and was approved by the regional ethics committee in Umeå, Sweden, by the division for medical research (Dnr 2010-371-31M) and by the head of the NUS Radiotherapy Department.
For our research, we chose to employ ‘quick’ ethnographic methods for our HCD research within the radiotherapy clinic, in order to maximize the efficiency of our fieldwork and to work within the ethical constraints of the hospital, which limited our ability to conduct direct interviews with patients. Ethnography is a regularly employed research method in design, used to gather information about users’ needs and preferences (Dourish, 2006). Ethnography can be understood as a way of “participating in people’s lives for an extended period of time, watching what happens, listening to what is said, asking questions – in fact, collecting whatever data are available to throw light on the issues that are the focus of the research” (Hammersley & Atkinson, 2007, p. 3). It is commonly used in HCD because of its emphasis on understanding the member’s point of view and their experiences (Dourish, 2006). The analytic contributions that ethnography can bring to design are rich, detailed accounts of human experience, as well as implications for design in the form of “consequential, profound, and direct guidance for how to think about user experience” (Dourish, 2007, p. 13). Furthermore, ethnography is particularly suited for focusing on the role of emotion in experience, which is well aligned with our interest in the relationship between patient experience and anxiety during cancer care.
Historically ethnography has been characterized by the long duration of its fieldwork, with a minimum of one year spent in the field, however, the growing costs of field research has placed demands upon research efficiency and productivity. Handwerker (2001) presents ‘quick ethnography’ as a means for collecting and analyzing high-quality ethnographic data in a much shorter timeframe, i.e., 90 days or less. Furthermore, this ‘quick ethnography’ approach enables researchers to gather rich data without direct interaction with the object of study (Handwerker, 2001). Using ‘quick ethnography’ enabled us to create a detailed analytical account of patient interactions within the radiotherapy clinic. We used patient observations and informal interviews with staff members to collect data about the different types of patient interactions that occur within this environment and the emotional responses expressed in relation to these interactions (Hammersley & Atkinson, 2007; Handwerker, 2001). We conducted our research in two phases, with the first phase establishing a baseline understanding of the processes involved in going through radiotherapy treatment, and the second phase focusing upon the patient experience within the clinic to identify problems within this context. We collected our data primarily through ethnographic field-notes and photographic documentation, and secondarily through self-reporting materials distributed to patients.
Method
In the first phase of our research, we spent two weeks shadowing the radiotherapy staff, a technique used to immerse ourselves into the lives of the staff in order to observe their behavior and experiences (McDonald, 2005). During this time, we learnt the step-by-step process of how radiotherapy treatment is planned and delivered. We focused on learning the roles of the various actors in this system and the requirements of the technologies they utilized, recording our findings using detailed field-notes. Observations were initiated in the Computed Tomography (CT) room where digital images of the patients’ tumors are taken by the CT nurses. We followed these files to the dose planning room, where doctors and the dose planning nurses work to map out the patient’s radiation treatment plan. Finally, we observed the treatment room nurses to understand how the patient’s individual dose plan is implemented. Within our field-notes, we noted each piece of technology and software used during the treatment process, and its use. We also fully documented the different roles that the staff members played in providing treatment to the patient, and their interactions with the different technologies. Finally, we documented the line of visibility within the treatment process, i.e., what was happening with the patient and what occurred behind-the-scenes among the staff (Emerson, Fretz, & Shaw, 1995; Marcus, 1998).
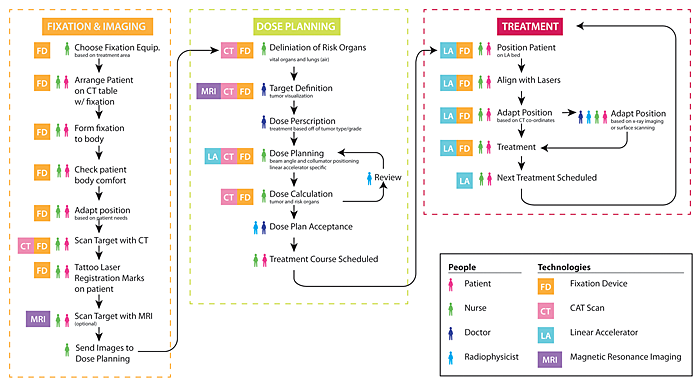
As part of our analysis, we visualized the radiotherapy process in a series of information diagrams (Stickdorn & Schneider, 2010). From our initial observations of 30 different staff members (24 nurses, 2 doctors, and 4 radiophysicists), and drawing on information collected from informal interviews with 12 of these individuals, we mapped out the radiation therapy workflow, noting where different technologies and staff are utilized in the planning and treatment process (Figure 1). The purpose of this map was to identify the different actors within the radiotherapy treatment process, paying close attention to the technologies involved and the level of influence that they play on the service being provided. Through this mapping, certain technologies, such as fixation devices, were discovered to play pivotal roles in the system, and influence the services provided by the radiotherapy clinic at every level of care.
Figure 1. Radiotherapy workflow – A multi-actor and technological environment.
(Click to enlarge this figure.)
In the second phase of our research, we spent our time focusing solely on the patient experience within the clinic. This required looking at the environment with a new lens. We used salience hierarchy to determine which data to record in our field-notes, focusing upon the commonalities and differences between individual patient experiences (Emerson et al., 1995; Wolfinger, 2002). Our rational for recording our observations using this approach was a response to the large numbers of patients being treated, per room, per day, each being handled in a similar manner.
The NUS radiotherapy clinic, which sees an average of 180 patients per day for radiation therapy, provides both curative and palliative treatments to individuals with a wide variety of cancers. We focused our observations upon the curative patient population, documenting the interactions of over 62 different patients within this environment. Radiotherapy with curative intention is generally delivered over a period of several weeks, with treatments occurring five days a week. This means that these patients have a high level of exposure to the treatment environment, and the interactions they have during their sessions can critically impact their experience of the service as a whole.
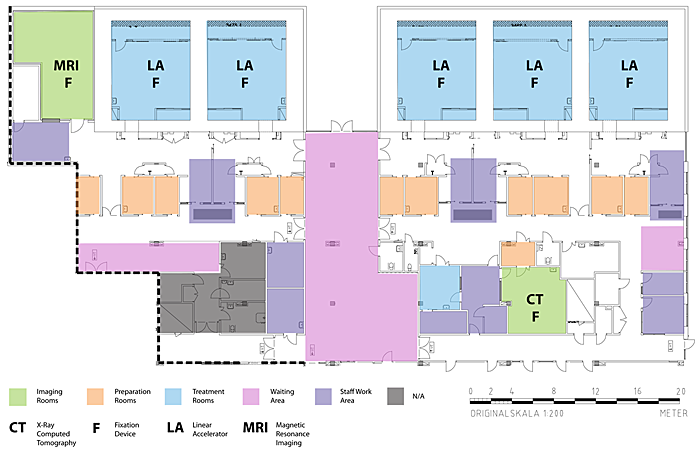
We conducted observations in every type of room in the clinic that the patient is exposed to during the treatment process in order to understand the different types of interactions the patients experienced in these different spaces (Figure 2). Our observations started in the waiting room, and followed patients through their treatment process, into the pre-treatment and treatment rooms. We took extensive field-notes about the characteristics of these spaces, studying the atmosphere, as well as the amount of time spent in each room, and we supplemented our notes with photographs. In addition, we also noted patient behaviors and actions in our field-notes, i.e., what they spent their time doing in each of these spaces.
Figure 2. Floor plan of the NUS radiotherapy clinic, noting the core technologies within these spaces.
(Click to enlarge this figure.)
After observing one patient having a panic attack associated with the fixation device, we immediately decided to conduct a more thorough investigation of this technology and its impact on patient experience. We closely observed patient interactions with this technology, and documented their expressions of emotions and physical reactions, i.e., laughing or crying. Additionally, we followed up any observations of extreme patient reactions with interviews of the care staff present during this experience to gather more information about the potential causes of the response. We also paid attention to the physical interactions between the patients and the technology, documenting the physical process of treatment that the patient goes through, i.e., how the body experiences treatment, using both field-notes and photographs.
To supplement the perspective we gained through our observations and to increase the likelihood that we were truly capturing the patient’s voice (due to our inability to conduct patient interviews), we distributed journals and cameras to a small group of patients (14 individuals in total) for them to verbally and pictorially document their experiences over the course of 5 weeks of treatment (see Figure 3 for an image of the materials). The journal contained open-ended questions about different aspects of treatment, ranging from their initial impressions to what they thought about during treatment. The narratives collected were used to supplement our observational findings and provide experiential details of what it is like to go through radiation treatment from a first-person perspective.
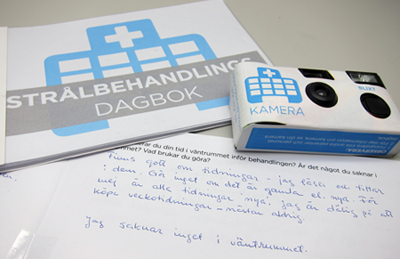
Figure 3. Daily journal and camera distributed to patients.
A common design approach would have been to empirically analyze our ethnographic data to create a set of short-term requirements or delimited implications for the design of technologies (Dourish, 2006). Such an approach was not appropriate as our aim was to provide a theoretical contribution to the design of technologies, with a broader scope and long-term impact (Blomberg, Giacomi, Mosher, & Swenton-Wall, 1993; Dourish, 2007). Thus, we used our richly detailed accounts of the patient experience to extract and examine the emotional components of their interactions within the clinic. We found that the deviant instances of treatment, i.e., where the treatment routine was disrupted by the patient, provided great insight into the conflicts that can occur within the radiotherapy process. In these cases, the patients became key informants for understanding the emotional experience of radiation therapy, and within this paper, the details of their treatment experiences are used to highlight the prevalence of anxiety within patients undergoing radiotherapy.
Site Specifics
The NUS radiotherapy clinic contains a wide variety of technologies that enable the healthcare staff to treat their patients. Linear accelerators (LA), imaging and dose calculation software, fixation devices, a magnetic resonance imaging (MRI) machine and a CT machine all play instrumental roles in providing treatment. Additionally, there are many different actors that play a role in treatment, from nurses, doctors and radiophysicists, to the patients and their family members. When a patient has been diagnosed with cancer and the oncologists determine that radiation therapy will be used as a method of treatment, the first step in the treatment process is to construct an individualized immobilization strategy for the patient. The immobilization strategy is selected based upon the type of tumor and the patient’s physical constraints. The selected strategy determines what position the patient will be in during their treatments and which standardized fixation devices will be utilized. These devices are used throughout the entire course of treatment in order to provide reproducible patient positioning during each treatment session.
The purpose of the fixation device is to immobilize the patients while they interact with the diagnostic imaging technologies, i.e., the CT and MRI, as well as the LA’s used to treat them. The images gathered through diagnostic imaging are used by the physicians to define the treatment area of the tumor, the specific treatment volume to be dosed with radiation, and the positioning of this volume in relation to skin marks or bony structures used for alignment during treatment. Planning of the treatment includes identification of optimal irradiation direction, shaping of the radiation fields, and dose calculation. The planning is performed by radiophysicists and trained nurses. Before radiation dosing can be administered to the patient, a simulation of the dosing is run on the computer so that the physician can approve the calculated dose distribution to the patient. The entire treatment planning process relies on absolute setup and position reproducibility.
Once the planning stage of treatment is complete, the patient is scheduled to begin their radiation therapy. Radiation treatments are given daily, for up to eight weeks, depending upon the type of tumor being treated. For example, most breast cancer patients receive an average of 25 treatments (5 weeks). These treatments can last anywhere from 5 minutes to 15 minutes depending upon the type of LA being used and the treatment area. Because of the recurring nature of this type of treatment, it is especially important to ensure that the experience is not stressful for the patient. Once a baseline understanding of the system was established, we focused our observations upon understanding the relationship between patients, nurses, and the technology. Since our initial findings highlighted the crucial importance of body positioning in radiation treatment and suggested that the technology used to immobilize patients could cause them emotional distress, we narrowed the focus of our observations down to patients with head, neck, and breast tumors, and the restrictive fixation devices that they interact with during radiotherapy.
Analysis and Insights
Design is multi-disciplinary in nature, as shown by the integration of ethnography into the HCD process; a method which originated within the field of anthropology (Dourish, 2006). In order to elucidate the impact of the fixation device upon patient experience and anxiety during radiotherapy, we decided to extend this multi-disciplinary nature further and draw on theory from the field of STS to help us analyze the relationship between this technology and the various actors interacting with it. We apply theory on actors, technological agency and use to our observations of the interactions that take place with the fixation device to map and understand the nature of the patient-technology interactions occurring within the radiotherapy clinic.
Firstly, this analysis looks closely at the importance of the fixation device in providing radiation treatment to cancer patients, and investigates patient immobilization as a result of the embedded social construct of the ‘passive patient’ within its design. Secondly, the strong emotional responses this restraint elicits from patients, and the consequential impact these emotions have upon treatment efficacy is explored. And thirdly, a comparison of patient interactions with this object to those of the nursing staff is employed to examine their disparate experiences with the fixation device and discuss the concept of ‘the user’ within medical technologies.
Immobilization and Power
The first interactions that a patient has with the staff of the NUS radiotherapy clinic after diagnosis is in their immobilization strategy appointment, where a fixation device is selected and the patient is scanned with the CT machine while under fixation (see Figure 4 for examples of different fixations). Although this interaction only occurs once, at the beginning of treatment, it can be a formative experience for the patients. Many different styles of fixation devices can be used for radiation therapy, each one designed to immobilize a different area of the body. These can range from immobilizing specific regions of the body to the entire patient. Face masks are used for treating head and neck tumors and immobilize only the head, while whole body vacuum bags are used to immobilize much larger regions of the body when other fixations are not appropriate.
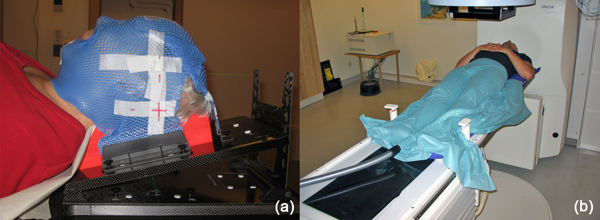
Figure 4. Image of fixation devices: (a) head fixation and (b) whole body vacuum bag fixation.
Patient positioning and immobilization is extremely important during radiotherapy. The sole focus of the fixation device is to provide reproducible patient positioning throughout the duration of the patient’s treatment regimen. Within this care environment, immobilization can be defined as the act of limiting movement through the fixation of a body part in order to facilitate treatment, and thus, cure the disease. Without proper immobilization, the patient is at risk of having a reduced cure probability due to complete or partially missed target volume, i.e., the tumor, for their radiation treatment, as well as an increase in adverse side effects due to accidental dosing of sensitive organs. The use of immobilization devices has been proven to significantly reduce errors in patient positioning, making this technology critical to providing treatment (Rosenthal et al., 2003). Radiation therapy treatment success is currently measured as being directly proportional to the level of immobilization of the patient’s body, i.e., the level of control over patient body movement (Gilbeau et al., 2001). At the same time, interaction with fixation devices requires patients to relinquish control over their physical movement, rendering them immobile and powerless.
Within healthcare, medical technologies are mainly perceived as instruments; tools that are employed for their ability to aid in providing treatment to patients. Researchers in the field of STS study the social influence these technologies can have beyond their functional capabilities. According to Akrich (1992), technological objects have the ability to enable or constrain human relations. Technologies can define the framework of the actions they enable, as well as the individuals they interact with and the space they inhabit. Consequently, technologies have the ability to attribute specific actions and responsibilities to their users, creating new roles or reinforcing existing ones (Akrich, 1992). Drawing on Stolterman’s (1999) argument that not only does “technology restrict and enable certain behavior,” but also “the way that it does this has a strong impact on how we will use the technology and how we will create a social entity around it” (p. 7). Taken together, these theories suggest that medical technologies can both constrain and frame the interactions that individuals have with them, influencing how they are used and how they are incorporated into the healthcare system.
Mol (2008) looks closely at the role of technologies in healthcare, and suggests that technologies which provide care are never neutral objects. Technologies made with the express purpose of contributing to improving lives are embedded with societal notions of what counts as an ‘improvement’, as well as what ‘treatment’ is and how it should be provided (Mol, 2008). The idea that medical technologies are imbued with social values is supported by Latour (2007), who suggests that all technological artifacts carry with them an inscribed set of behaviors that are embedded within the technology itself, as a direct result of it being a created entity, and according to Grint and Woolgar (1992), “a technical object can only exist as a result of prior social constructions and social actions” (p. 373). Tying the theory that technology is embedded with social values together with the theory that technologies enable or constrain our actions, we begin to understand that as created artifacts, medical technologies are embedded with our social values, and as such, these ‘instruments’ have much more power than initially perceived.
Since technologies can be embedded with societal values, even unintentionally, it becomes important for our research into patient experiences with medical technologies to investigate the social roles and values placed upon the patient within healthcare. One article reviewing the role of wellbeing in healthcare argues that “in the relationship between healthcare providers and patients, providers dominate” (Dubberly, Mehta, Evenson, & Pangaro, 2010, p. 56). Extending this, Mol (2008) emphasizes this position in the quote, “as patients we are treated as objects and made passive” (p. 6). According to the social script of illness behavior put forth by Parsons (1951, p. 437), the sick individual has an ‘obligation’ to go to a doctor and ‘cooperate’ with him in order to get better. Within this ‘sick role’ construct, healthcare professionals take control of diagnosing and treating the patient’s health problems, while the individual seeking medical care takes on the role of the ‘patient’, allowing the ‘professional’ to tell them what to do, and how to do it, in order to get better. These roles have become so deeply embedded within the healthcare system that it has been written into medical language and metaphor. Professionals ‘care for’ patients. Their proposals are ‘prescriptions’ and ‘physician’s orders’, and patients who do not take their medicines or agree to their treatment suggestions are considered ‘not in compliance’ (Dubberly et al., 2010). This suggests that the patient is often placed in the role of ‘passive receiver’ of the medical expertise provided by healthcare professionals and that this unequal distribution of power is still written into many patient experiences. If medical technologies are designed by individuals adhering to the script of the patient as passive subject rather than active participant, one can expect that these technologies will act on the patient in the same way.
Our observations of the immobilization inherent in patient interactions with fixation devices, when interpreted through the lens that technology is embedded with social values, supports Mol’s (2008) and Dubberly et al.’s (2010) concept of the passive patient. The restrictive nature of this technology places patients in a disempowered position during radiotherapy, where they become passive recipients of treatment. It is interesting to note that the fixation device and immobilization are not limited to the sphere of radiotherapy. Many medical technologies require patients to be immobile during their use. Currently all diagnostic imaging technologies, from x-ray and ultrasound to CT and MRI, require some degree of patient immobility in order for them to function properly. Since tumor imaging plays a crucial role in targeted radiation therapy it is important, understandably, during radiotherapy also. If we extend our insights about the fixation device to medical technology as a whole, we suggest that many medical technologies are embedded with the social construct of the ‘passive patient’, and the action space that they afford these individuals is narrow and constrained to the role of ‘receiver of treatment’ instead of ‘active participant’ within healthcare.
Anxiety and Accuracy
While fixation devices were created to help increase the accuracy of radiation treatment, they have been found to trigger the unexpected effect of anxiety in many of the patients interacting with them. Medical research has found that reproducibility during radiotherapy of head and neck tumors has been significantly improved by face masks, however, the temporary fixation of the head and neck region is also shown to induce situational anxiety in the patients, and as a result reduces the overall compliance of this technique (Adamietz, Kremmin, & Emminger, 1991). Our observations of patient interactions with fixation devices fully support these medical findings.
During our ethnographic fieldwork in the radiotherapy clinic, we observed one neck cancer patient going through the process of being fitted with a face mask and categorized this individual as a critical informant based on her discussions with the nurses about how the mask had triggered feelings of anxiety and claustrophobia, despite not normally having any problems with enclosed spaces. This patient explained how she had used deep breathing relaxation techniques to stay calm and not panic during her fitting appointment. Since the physical restraint caused by the face mask can continue to cause anxiety in patients throughout the duration of treatment, in subsequent radiation treatment appointments, we observed several instances where the nurses made adjustments to the masks to make them more tolerable, such as cutting eye openings so patients can keep their eyes open during treatment. The strong impact these minor alterations make on the patient experience is made apparent in the journal of a patient who reported suffering from claustrophobia during treatment. She described her experience with the face mask in the following two statements:
I had a panic attack the first time. I could not handle being trapped in the mask. Then the staff modified the mask so that it didn’t put pressure on the neck. The next day I asked to them to make eye holes for me, which they did. Now it’s ok.
Before my mask was modified I panicked. It was not easy to breathe normally.
In addition to mask alterations, patients are given a panic button to hold in their hand during their radiation treatments. When pressed, this button notifies the nurses that something is wrong and that they need to stop the radiation. The presence of devices designed for patients to be able to communicate that they are distressed during treatment demonstrates how common this type of reaction is in the patient population.
While the stories above are subtle examples of how patients and nurses have already begun to counteract the anxiety inducing experience of the fixation device, sometimes the emotional impact cannot be mediated. During our fieldwork, we observed one extreme case where the negative emotional impact of the fixation device was so strong that it caused the patient to seek alternate treatment. This individual was observed during her initial fixation device fitting and CT scanning appointment, where she was visibly agitated and crying, requiring continuous verbal support from the nursing staff. At the end of her appointment, the patient requested to see what it would be like to go through radiation treatment with the fixation device, and she was allowed to test this out in one of the treatment rooms. In a follow-up interview with the nurses who had worked with this patient, we learned that the patient suffered from claustrophobia and had experienced a severe panic attack in response to her interactions with the fixation device. The combined effect of immobilization and the close proximity of the LA in the treatment room had induced an overwhelming fear response in the patient. The end result of this experience was that the patient refused to undergo radiation therapy and opted for a more aggressive surgery instead to remove her cancer.
While radiation therapy may have been the best treatment option for this patient’s cancer, for the patient as an individual, a mastectomy (complete removal of the breast) was the best option for her personal and physical wellbeing during treatment. The patient decided that the anxiety and psychological stress of daily radiation therapy for five weeks would have been much more detrimental to her cancer care than the single surgery required to remove the cancerous tumor, despite it being a more aggressive and invasive treatment than necessary. The strong emotional reaction of this patient in response to the fixation device had a direct and measurable impact upon the function of the device, resulting in the technology being rendered unusable for treatment.
The observation that fixation devices can trigger patient anxiety is supported by the research of Clover et al. (2011), who found that:
The [fixation device] mask often engenders patient anxiety to an extent which is not only distressing for the patient but also affects the operation of the department through disruption to treatment, longer waiting times in clinic for other patients and distress for staff. (p. 1335)
Furthermore, their research shows that head and neck patients who experience fear of enclosed spaces, fear of face being covered up, fear of movement restriction, and/or have ever had an anxiety attack are significantly more likely to disrupt their radiotherapy treatment session due to anxiety (Clover et al., 2011). As our example of the patient with claustrophobia has shown, this anxiety can do more than just disrupt treatment; it can make treatment with the fixation device impossible.
The strong emotional responses in patients using a fixation device are consistent with other research that shows that feelings of vulnerability and loss of control have been shown to trigger anxiety and stress responses (Walding, 1991). Emotions help individuals establish their position within their environment, pulling them towards what they regard as beneficial, and pushing them away from what they see as detrimental. Emotion always involves an assessment of how an event may harm or benefit a person, with three possible outcomes: beneficial, harmful, and not relevant (Desmet, 2003). Immobilization is seen as a complex stressor, with both physiological and psychological components to it, and it is one of the most frequently employed laboratory test models of stress (Kvetnansky & McCarty, 2000). Humans instinctively respond to immobilization, sensing restraint as a physical threat (Plutchik, 1994).
The fixation device has been designed in consideration for its use, operation, and management, but the interactions that can influence more indirect responses such as emotions have generally been disregarded. This patient’s fear response to the treatment technology shows us one example of the conflict that can occur between medicine’s best treatment and its best care. According to Mol (2008), “the scientific tradition that is currently most prominent in healthcare - clinical epidemiology - has not been designed to deal with unexpected effects of interventions” (p. 86). In this case, the unexpected effect of the fixation device is patient anxiety. Not only can the interactions of the fixation device unintentionally trigger patient anxiety, but also this anxiety can lead to a decrease in efficacy of the treatment being given. It can be questioned whether the emotional distress caused by the fixation device ultimately offsets any treatment benefits gained.
The Implicated Actor
As our examples have shown, the fixation device can trigger patient anxiety on a variety of different levels but the question remains, why is this situational anxiety not accounted for in the design of this technology? Patient positioning is arguably the most important aspect of radiation therapy, so how do we end up with devices that were designed to improve treatment accuracy, but through use, result in side effects that hinder their own function? The answer to these questions lies in understanding how this technology constructs different action spaces and responsibilities for the different groups of individuals that interact with it.
The fixation device is designed to enable the healthcare staff to accurately position patients in a reproducible manner. For them, the fixation device is a tool that allows them to make connections between the tumor visualizations captured by the CT machine, and the calibrated radiation output given by the LA machine. Without the fixation device, patient positioning is extremely difficult to replicate, and results in radiation dosages that are more distributed to ensure that the tumor is properly dosed, i.e., the way it was done in the past before the invention of targeted radiotherapy. Fixation devices have been designed as useful and empowering tools for the healthcare staff responsible for correctly positioning patients during treatment, and it does this job extremely well.
From the examples gathered in our case study, we see patient interactions with the fixation device as being characterized by physical restraint, disempowerment, and strong negative emotional responses. We suggest that these vastly different experiences with the fixation device are due to the societal roles that are embedded in the design of this technology. Cowan’s (1987) research on user-technology relations suggests that there are many different types of users. With medical technologies, the term ‘user’ can be used to describe the nurses and medical professionals who operate the technology, the patients who interact with it, the health care administrators who purchase it, to name just a few. Using Friedman’s (1989) typology of users, we see that ‘users’ fall into many different categories, however, the ‘end users’, i.e., the operators of the technology, are the only individuals for whom direct interactions with the technology have been actively designed.
We suggest that in the case of the fixation device, the nurses and doctors responsible for the operation of the equipment are the only individuals that have been defined as ‘end users’ during the development of this technology. Despite their direct interactions with the technology, patients can unfortunately be categorized as ‘implicated actors’ for this technology; individuals who are silent but affected by the action of the technology (Clarke, 1998). According to Clarke (2005) there are two different categories of implicated actors, “those not physically present but who are discursively constructed and targeted by others” and “those who are physically present but who are generally silenced/ignored/made invisible by those in power” (p. 46). The cancer patients we have studied within this paper are both physically present and directly interacting with the technology, and yet at the same time, they are silent in these interactions, rendered powerless by the technology. We speculate that the observed lack of consideration for the patient as an active user of this technology is directly responsible for the negative emotional responses elicited by these individuals during their interactions with the fixation device.
The fixation device demonstrates how two individuals interacting with the same object at the same time can interact with and experience it in two drastically different ways. The fixation device is a tool which aids healthcare staff in actively providing radiation treatment to the patient, with the end goal of curing cancer. At the same time, patients’ interactions with this technology render them passive and removed from control. If technology defines the action spaces of the actors that interact with it, the examples provided in this paper show that the action space of the fixation device is definitely not equal for all actors. While the fixation device can open up a wide area of treatment possibilities for healthcare professionals, it also closes down the physical action space of the patient. We argue that the power dichotomy seen in patient versus provider interactions with this device is a direct result of this technology being embedded with the social construct of the ‘passive patient’, and it continually reinforces them through its actions.
Opening the Solution Space
With the case of the fixation device, we have found that patient anxiety can arise from immobilization and restraint. In turn, this anxiety can have a detrimental impact on both patient experience and radiotherapy treatment accuracy. Taken together, we argue that the fixation device is a situational trigger for patient anxiety within this environment. Going back to our starting discussion around person-centered care, we recall that the majority of interventions surrounding patient anxiety are focused upon coping techniques, and that little attention is placed upon creating interventions to impact the triggers of this anxiety.
Our design research calls attention to these triggers, and suggests that the solution space of PCC should be expanded beyond its focus on cancer patient coping to encompass the situational triggers of anxiety as well, especially those that are embedded within the healthcare system. Patients already experience anxiety as a consequence of living with cancer; their care experience should not make this worse. As we have seen from the examples in this paper, patients are willing to tolerate both physical and emotional discomfort during treatment in order to avoid death. It is only under extreme emotional duress that an individual will seek out alternate conditions for treatment, choosing a more drastic or potentially less successful alternative. According to Mol (2008), when given a choice between having a potentially lethal disease and a treatment that could allow you to live for a long time, most patients say “I have no choice” (p. 40). This desire to live often overshadows all other aspects of the treatment experience. While patients may be willing to tolerate a high level of physical and emotional discomfort in order to live, this does not mean that we should forgo consideration for the more subjective, emotional qualities of the patient experience in the quest for providing the best treatment possible.
Human-centered design is an approach that integrates multidisciplinary expertise to enhance human wellbeing and empower people, and it leads to systems, machines, products, services and processes which are physically, perceptually, cognitively and emotionally intuitive to use. Due to its broad scope, HCD implements a holistic approach and works across of a range of different design inputs to attack the problems that it identifies through research into human needs. We suggest that HCD is a useful approach to employ in tackling the complex issue of patient anxiety within the radiotherapy clinic, and healthcare at large.
At the most basic level, based on our research findings of the link between patient anxiety and the fixation device, we suggest that design methods should be employed to redesign the fixation device, or even the alignment system within the treatment room, so that it empowers both the nurses and the patients. Radiotherapy nurses have already begun to explore this design space through their in situ adjustments to the fixation masks. As we know, these nurses currently play a critical role in aligning and adjusting the patient’s body during radiotherapy. But what would happen if the patient was given an active role in their positioning? One can imagine that if the patient understood how their body should be aligned, that they would be much more capable of moving their body into the correct position than the nurses. We suggest that it is just as possible to design a technology that facilitates relaxation in the patient and supports them in finding the optimal body position for treatment than it is to design one that restrains and immobilizes. An object-focused design approach could be implemented to not only redesign the fixation device, but also re-envision the process of fixation.
At the same time we have seen that the fixation device plays a key role in the radiotherapy treatment process. The restraint of the fixation device allows for reproducible patient positioning, a process which is an integral part of the radiotherapy treatment process, and may not be able to be designed away. In the context of healthcare, service-focused design methods concentrate upon the delivery, dissemination, and implementation of care, i.e., the servicescape (Lee, 2011). A service focused design approach could be implemented in a variety of ways to mediate the situational stress caused by the fixation device. Potential solutions could range from a service that allows the patients to connect with the fixation devices outside of the clinic environment to familiarize them with the experience in a comfortable setting, to interventions within the treatment room aimed at distracting the patient from their emotional distress. Individuals from within healthcare, such as Dr. Nicholas LaRusso of the Mayo Clinic’s Center for Innovation, have already been advocating the idea that service-focused design is one way to reform healthcare. LaRusso suggests that improving the ways we deliver new technologies, diagnostic tests, and therapeutics to patients will increase their effectiveness (Design and Social Enterprise Case Series, 2011).
Design implemented at a higher level, could focus on shifting social perspectives on the role of patients within healthcare from implicated actors to powerful resources and key users within this system, a perspective already being vocalized from within this community through the PCC movement. Transformation-focused design approaches apply user-centered design principles to large scale systems and services to activate cultural change within organizations and communities (Burns, Cottam, Vanstone, & Winhall, 2006; Sangiorgi, 2011). Transformation-focused design methods could be used to advocate for human-centered design culture within healthcare institutions and companies producing medical technologies to create new policies and work structures that support the shift to person-centered care.
Taken together, HCD is capable of looking holistically at the problem of patient fixation to discover new solutions spaces for dealing with the anxiety triggered by this particular technology. While this paper has focused solely on one technology within a radiotherapy clinic, we propose that taking this approach to studying the designable triggers behind patient anxiety or other negative emotions (i.e., the ones that are caused by the healthcare environment) will greatly broaden the scope of PCC, transforming it from a responsive practice to a pre-emptive one.
Conclusions
There is a need to rethink the patient experience within healthcare. It is well known that patients can experience anxiety during their interactions with medical environments, and healthcare providers are increasingly realizing that what they’re offering is not enough to meet the needs of their patients. Focus on the scientific method and evidence-basing within medicine has led to a singular focus on disease rather than a focus on the patient as a whole. According to Norman (2008), “[With] so many numbers, we lose sight of the person. Scientists measure what they can measure and pronounce the rest to be unimportant. But the most important parts of life are qualitative” (p. 15). The negative impact of this biomedical approach has been recognized throughout nursing research, and much is being done from within this field to advocate patient centered care, with the belief that this approach will lead to improved quality of life and personal wellbeing during illness.
In looking at the incidence of anxiety within cancer patients, advocates of PCC have employed many methods for mediating this emotion through patient empowerment. In analyzing the solution space of this problem we highlight how the person-centered approach within nursing focuses on patient coping techniques. These psychosocial interventions are limited to the realm of dealing with the condition of anxiety after it has already been expressed. This paper demonstrates that design can be a useful tool to broaden this solution space through application of new perspectives to the conceptualization and identification of the problem of patient anxiety and its situational triggers in healthcare experiences.
In addition, this paper has shown how HCD can successfully draw on methods and theories from different research fields and integrate them into its own research and analysis techniques. The case study demonstrates how ‘quick’ ethnographic methods were implemented to explore the complex phenomenon of patient experience and provide rich data on spaces where conflicts arise within cancer treatment. This methodology enables designers to conduct exploratory field research that can identify meaningful and contextualized ‘user’ problems. Furthermore, the application of STS theory was crucial to the analysis and contextualization of our findings involving patient anxiety and its link to the fixation device. This paper advocates that the multi-disciplinary nature of HCD research is integral to its ability to identify problems and analyze them from many different perspectives, and through this ‘border-crossing’ open up solution spaces that were previously well-defined.
Overall, this paper suggests that human-centered design thinking and processes should be implemented within healthcare, with designers working in conjunction with medical providers and patients to support PCC. However, this paper only presents one half of the design process; the front-end research into patients’ needs and experiences. In order to impact patient anxiety within the radiotherapy clinic, this work needs to be taken from research into design practice, where design interventions are implemented within the clinic and their effects assessed. Suggestions for future directions for this work are not limited to design interventions. We have studied only one small facet of patient experience within cancer treatment, i.e., the fixation device, and the insights gathered in this research suggest that there are many other areas that can play an influential role in the complex problem of patient anxiety. We suggest that the open, holistic perspective of HCD is ideal for finding new ways to generate the frame-shift required to think beyond ‘the cure’ to person-centered care and wellbeing.
Acknowledgments
We would like to thank Christina Andersson, M.D., Per Bergström, M.D. and David Edvardsson, Ph.D., for their advisory roles at the initiation of this project, with special thanks to Christina for her support with enrolling patients in the journal aspect of our research. We would also like to thank all of the NUS radiotherapy clinic staff and patients for their active participation in this study. This research is funded by the EU Structural foundation Objective 2, North Sweden, and the Cancer Research Foundation of Northern Sweden.
References
- Adamietz, I. A., Kremmin, B., & Emminger, A. (1991). A modified facial mask device for the radiotherapy of head-neck tumors. Strahlenther Onkol, 167(8), 477-479.
- Akrich, M. (1992). The de-scription of technical objects. In W. E. Bijker, & J. Law (Eds.), Shaping technology/building society: Studies in sociotechnical change (pp. 205-224). Cambridge, MA: The MIT Press.
- Andersen, B. L., Karlsson, J. A., Anderson, B., & Tewfik, H. H. (1984). Anxiety and cancer treatment: Response to stressful radiotherapy. Health Psychology, 3(6), 535-551.
- Stickdorn, M., & Schneider, J. (2010). This is service design thinking: Basics, tools, cases. Amsterdam, the Netherlands: BIS Publishers.
- Andrykowski, M. A. (1990). The role of anxiety in the development of anticipatory nausea in cancer chemotherapy: A review and synthesis. Psychosomatic Medicine, 52(4), 458-475.
- Blomberg, J., Giacomi, J., Mosher, A., & Swenton-Wall, P. (1993). Ethnographic field methods and their relation to design. In D. Schuler & A. Namioka (Eds.), Participatory design: Principles and practices. (pp. 123-155). Hillsdale, NJ: Lawrence Erlbaum Associates.
- Brooker, D. (2007). Person-centred dementia care: Making services better. London, UK: Jessica Kingsley.
- Brown, L. F., Kroenke, K., Theobald, D. E., Wu, J., & Tu, W. (2010). The association of depression and anxiety with health-related quality of life in cancer patients with depression and/or pain. Psycho-Oncology, 19(7), 734-741.
- Burns, C., Cottam, H., Vanstone, C., & Winhall, J. (2006). RED paper 02: Transformation design. London, UK: Design Council.
- Cameron, L. D., Leventhal, H., & Love, R. R. (1998). Trait anxiety, symptom perceptions, and illness-related responses among women with breast cancer in remission during a tamoxifen clinical trial. Health Psychology, 17(5), 459-469.
- Carlson, L. E., & Bultz, B. D. (2003). Benefits of psychosocial oncology care: Improved quality of life and medical cost offset. Health and Quality of Life Outcomes, 1, 8. doi: 10.1186/1477-7525-1-8
- Clarke, A. (1998). Disciplining reproduction: Modernity, American life sciences, and the problem of sex. Berkeley, CA: University of California Press.
- Clarke, A. (2005). Situational analysis: Grounded theory after the postmodern turn. Thousand Oaks, CA: Sage Publications.
- Clover, K., Oultram, S., Adams, C., Cross, L., Findlay, N., & Ponman, L. (2011). Disruption to radiation therapy sessions due to anxiety among patients receiving radiation therapy to the head and neck area can be predicted using patient self-report measures. Psycho-Oncology, 20(12), 1334-1341.
- Cowan, R. S. (1987) The Consumption Junction: A proposal for research strategies in the sociology of technology. In W. E. Bijker, T. P. Hugher, & T. J. Pinch (Eds.), The Social Construction of Technological Systems: New Directions in the Sociology and History of Technology. Cambridge, MA: MIT Press.
- Dale, W., Bilir, P., Han, M., & Meltzer, D. (2005). The role of anxiety in prostate carcinoma: A structured review of the literature. Cancer, 104(3), 467-478.
- Design and Social Enterprise Case Series (2010). Mayo clinic: Design thinking in health care. New York, NY: Yale School of Management. Retrieved January 15, 2011, from http://nexus.som.yale.edu/design-mayo/
- Desmet, P. M. A. (2003). A multilayered model of product emotions. The Design Journal, 6(2), 4-13.
- Dourish, P. (2006). Implications for design. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (pp. 541-550). New York, NY: ACM.
- Dourish, P. (2007). Responsibilities and implications: Further thoughts on ethnography and design. In Proceedings of the Conference on Designing for User eXperiences (Article No. 25). New York, NY: ACM.
- Dubberly, H., Mehta, R., Evenson, S., & Pangaro, P. (2010). Reframing health to embrace design of our own well-being. Interactions, 17(3), 56-63.
- Edvardsson, D., Sandman, P. O., & Rasmussen, B. (2006). Caring or uncaring – Meanings of being in an oncology environment. Journal of Advanced Nursing, 55(2), 188-197.
- Edvardsson, D., Sandman, P. O., & Rasmussen, B. (2008). Swedish language person-centred climate questionnaire – patient version: Construction and psychometric evaluation. Journal of Advanced Nursing, 63(3), 302-309.
- Emerson, R. M., Fretz, R. I., & Shaw, L. L. (1995). Writing ethnographic fieldnotes (1st ed.). Chicago, IL: University of Chicago Press.
- Forester, B. M., Kornfeld, D. S., & Fleiss, J. (1978). Psychiatric aspects of radiotherapy. The American Journal of Psychiatry, 135(8), 960-963.
- Friedman, A. L., & Cornford, D. S. (1989). Computer systems development:history, organization, and implementation. Chichester: Wiley.
- Gilbeau, L., Octave-Prignot, M., Loncol, T., Renard, L., Scalliet, P., & Grégoire, V. (2001). Comparison of setup accuracy of three different thermoplastic masks for the treatment of brain and head and neck tumors. Radiotherapy and Oncology, 58(2), 155-162.
- Greer, J. A., Pirl, W. F., Park, E. R., Lynch, T. J., & Temel, J. S. (2008). Behavioral and psychological predictors of chemotherapy adherence in patients with advanced non-small cell lung cancer. Journal of Psychosomatic Research, 65(6), 549-552.
- Grint, K., & Woolgar, S. (1992). Computers, guns, and roses: What’s social about being shot? Science, Technology & Human Values, 17(3), 366-380.
- Hammersley, M., & Atkinson, P. (2007). Ethnography: Principles in practice (3rd ed.). London, UK: Routledge.
- Handwerker, W. P. (2001). Quick ethnography: A guide to rapid multi-method research. Walnut Creek, CA: AltaMira Press.
- IDEO. (2011). Human-centered design toolkit: An open-source toolkit to inspire new solutions in the developing world. Chicago, IL: IDEO.
- Kvetnansky, R., & McCarty, R. (2000). Immobilization stress. In G. Fink (Ed.), Encyclopedia of stress (Vol. 2, pp. 503-506). San Diego, CA: Academic Press.
- Kvåle, K., & Bondevik, M. (2008). What is important for patient centred care? A qualitative study about the perceptions of patients with cancer. Scandinavian Journal of Caring Sciences, 22(4), 582-589.
- Latini, D. M., Hart, S. L., Knight, S. J., Cowan, J. E., Ross, P. L., Duchane, J., & Carroll, P. R. (2007). The relationship between anxiety and time to treatment for patients with prostate cancer on surveillance. The Journal of Urology, 178(3), 826-832.
- Latour, B. (2007). Reassembling the social: An introduction to actor-network-theory. New York, NY: Oxford University Press.
- Lee, S. (2011). Evaluating serviceability of healthcare servicescapes: Service design perspective. International Journal of Design, 5(2), 61-71.
- Marcus, G. E. (1998). Ethnography through thick and thin. Princeton, NJ: Princeton University Press.
- McDonald, S. (2005). Studying actions in context: A qualitative shadowing method for organizational research. Qualitative Research, 5(4), 455-473.
- Mol, A. (2008). The logic of care: Health and the problem of patient choice. London, UK: Routledge & Kegan Paul.
- Nandini, V., Sridhar. C. N., Usharani, M. R., Kumar, J. P., & Salins, N. (2011). Incorporating person centred care principles into an ongoing comprehensive cancer management program: An experiential account. Indian Journal of Palliative Care, 17(4), 61-67.
- Norman, D. (2008). The way I see it: A fetish for numbers. Interactions, 15(2), 14-15.
- Parsons, T. (1951). The social system. London, UK: Routledge & Kegan Paul.
- Penrod, J., Yu, F., Kolanowski, A., Fick, D. M., Loeb, S. J., & Hupcey, J. E. (2007). Reframing person-centered nursing care for persons with dementia. Research and Theory for Nursing Practice, 21(1), 57-72.
- Plutchik, R. (1994). The psychology and biology of emotion. New York, NY: Harper Collins College Publishers.
- Rosenthal, S. A., Roach, M. 3rd, Goldsmith, B. J., Doggett, E. C., Pickett, B., Yuo, H. S.,… Ryu, J. K. (1993). Immobilization improves the reproducibility of patient positioning during six-field conformal radiation therapy for prostate carcinoma. International Journal of Radiation Oncology, Biology, Physics, 27(4), 921-926.
- Sackett, D. L., Rosenberg, W. M. C., Gray, J. A. M., Haynes, R. B., & Richardson, W. S. (1996). Evidence based medicine: What it is and what it isn’t. British Medical Journal, 312(7023), 71-72.
- Sangiorgi, D. (2011). Transformative services and transformation design. International Journal of Design, 5(2), 29-40.
- Stark, D. P. H., & House, A. (2000). Anxiety in cancer patients. British Journal of Cancer, 83(10), 1261-1267.
- Stiefel, F., & Razavi, D. (1994). Common psychiatric disorders in cancer patients. II. Anxiety and acute confusional states. Supportive Care In Cancer: Official Journal Of The Multinational Association Of Supportive Care In Cancer, 2(4), 233-237.
- Stolterman, E. (1999). Technology matters in virtual communities. ACM SIGGROUP Bulletin, 20(2), 7-9.
- Teunissen, S. C. C. M., de Graeff, A., Voest, E. E., & de Haes, J. C. J. M. (2007). Are anxiety and depressed mood related to physical symptom burden? A study in hospitalized advanced cancer patients. Palliative Medicine, 21(4), 341-346.
- Walding, M. F. (1991). Pain, anxiety and powerlessness. Journal of Advanced Nursing, 16(4), 388-397.
- Wolfinger, N. H. (2002). On writing fieldnotes: Collection strategies and background expectancies. Qualitative Research, 2(1), 85-95.